FIBRINOLYTICS (Thrombolytics):
These are drugs used to lyse thrombi/clot to re-canalize occluded blood vessels (mainly coronary artery).
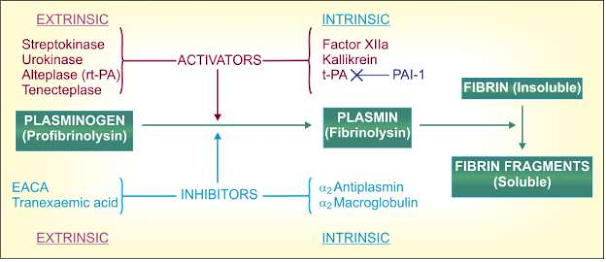
They are therapeutic rather than prophylactic and work by activating the natural fibrinolytic system.
The plasminogen-plasmin system
t-PA-Tissue plasminogen activator; rt-PA-Recombinant t-PA; PAI-1 Plasminogen activator inhibitor-1
The clinically important fibrinolytics are:
- Streptokinase
- Urokinase
- Alteplase (rt-PA)
- Reteplase
- Tenecteplase
Streptokinase:
Obtained from hemolytic Streptococci group C, it is the first fibrinolytic drug to be used clinically, but is not employed now except for considerations of cost.
Streptokinase is inactive as such; combines with circulating plasminogen molecules to form an activator complex which then causes limited proteolysis of other plasminogen molecules to generate the active enzyme plasmin.
It is non-fibrin specific, i.e. activates both circulating as well as fibrin bound plasminogen. Therefore, it depletes circulating fibrinogen and predisposes to bleeding.
Compared to newer more fibrin-specific tissue plasminogen activators (alteplase, etc.) it is less effective in opening occluded coronary arteries, and causes less reduction in MI related mortality.
There are several other disadvantages as well with streptokinase.
Antistreptococcal antibodies due to past infections inactivate considerable fraction of the initial dose of Stk.
A loading dose therefore is necessary.
Plasma t½ is estimated to be 30–80 min.
Stk is antigenic—can cause hypersensitivity reactions; anaphylaxis occurs in 1–2% patients.
It cannot be used second time due to neutralization by antibodies generated in response to the earlier dose.
Fever, hypotension and arrhythmias are reported.
However, being less expensive, it is still used in resource poor areas, but not in Europe or USA.
Urokinase:
It is an enzyme isolated from human urine; but commercially prepared from cultured human kidney cells.
It activates plasminogen directly and has a plasma t½ of 10–15 min.
It is non-antigenic.
Fever occurs during treatment, but hypotension and allergic phenomena are rare.
Urokinase is indicated in patients in whom streptokinase has been given for an earlier episode, but is seldom used now.
Alteplase (recombinant tissue plasminogen activator (rt-PA):
It is produced by recombinant DNA technology from human tissue culture, it is moderately specific for fibrin-bound plasminogen, so that circulating fibrinogen is lowered only by ~ 50%.
It is rapidly cleared by liver and inactivated by plasminogen activator inhibitor-1 (PAI-1).
The plasma t½ is 4–8 min.
Because of the short t½, it needs to be given by slow i.v. infusion and often requires heparin co-administration.
It is non-antigenic, but nausea, mild hypotension and fever may occur.
It is expensive.
Reteplase:
It is a modified form of rt-PA that is longer acting, but somewhat less specific for fibrin-bound plasminogen.
The longer duration of action enables bolus dose administration (10 mg over 10 min repeated after 30 min).
Tenecteplase:
This genetically engineered substitution mutant of native t-PA has higher fibrin selectivity, slower plasma clearance (longer duration of action) and resistance to inhibition by PAI-1.
It is the only fibrinolytic agent that can be injected i.v. as a single bolus dose over 10 sec, while alteplase requires 90 min infusion.
This feature makes it possible to institute fibrinolytic therapy immediately on diagnosis of ST segment elevation myocardial infarction (STEMI), even during transport of the patient to the hospital.
Several randomized multicentric trials have assessed its efficacy in STEMI and found it to be at least equally efficacious to alteplase.
Risk of noncerebral bleeding may be lower with tenecteplase, but cranial bleeding incidence is similar.
Uses of fibrinolytics:
1. Acute myocardial infarction is the chief
2. Deep vein
3. Pulmonary
4. Peripheral arterial occlusion
5. Stroke