Acute & Chronic gout
OBJECTIVE
At the end of the class the students will be able to
• Explain acute gout
• Briefly explain clinical presentation of acute gouty arthritis and uric acid nephrolithiasis
Gout
• Gout is diagnosed clinically by symptoms rather than laboratory tests of uric acid.
• In fact, asymptomatic hyperuricemia discovered incidentally generally requires no therapy because many individuals with hyperuricemia will never experience an attack of gout.
• These patients should still be encouraged to implement lifestyle measures to reduce serum urate concentrations.
Clinical Presentation
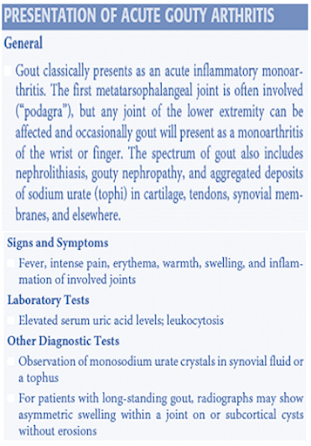
ACUTE GOUTY ARTHRITIS
• A classic acute attack of gouty arthritis is characterized by rapid and localized onset of excruciating pain, swelling, and inflammation.
• The attack is typically monarticular at first, most often affecting the first metatarsophalangeal joint (great toe) and then, in order of frequency, the insteps, ankles, heels, knees, wrists, fingers, and elbows.
• In one half of initial attacks, the first metatarsophalangeal joint is affected, a condition commonly referred to as podagra.
Clinical Manifestations of Gout
• Up to 90% of patients with gout will experience podagra at some point in the course of their disease.
• Atypical presentations of gout also occur. For elderly patients, gout can present as a chronic polyarticular
arthritis that can be confused with rheumatoid arthritis or osteoarthritis.
• Additionally, theonset of gout may be less dramatic than the typical acute attack and have fewer clinical findings.
• Multiple small joints in the hands may be involved, especially in elderly women.
• The predilection of acute gout for peripheral joints of the lower extremity is probably related to the low temperature of these joints combined with high intraarticular urate concentration.
• Synovial effusions are likely to occur transiently in weight-bearing joints during the course of a day with
routine activity.
• At night, water is reabsorbed from the joint space, leaving behind a supersaturated solution of monosodium urate, which can precipitate attacks of acute arthritis.
• Attacks generally begin at night with the patient awakened from sleep by excruciating pain.
• The development of crystal-induced inflammation involves a number of chemical mediators causing vasodilation, increased vascular permeability, complement activation, and chemotactic activity for polymorphonuclear leukocytes.
• Phagocytosis of urate crystals by the leukocytes results in rapid lysis of cells and a discharge of lysosomal and proteolytic enzymes into the cytoplasm.
• The ensuing inflammatory reaction is associated with intense joint pain, erythema, warmth, and swelling. Fever is common, as is leukocytosis.
• Untreated attacks may last from 3 to 14 days before spontaneous recovery.
• Although acute attacks of gouty arthritis may occur without apparent provocation, a number of conditions may precipitate an attack.
• These include stress, trauma, alcohol ingestion, infection,surgery, rapid lowering of serum uric acid by ingestion of uric acid-lowering agents.
• Other crystal-induced arthropathies that may resemble gout on Clinical Presentation are caused by calcium pyrophosphate dihydrate crystals (pseudogout) and calcium hydroxyapatite crystals, which are associated with calcific periarthritis, tendinitis, and arthritis.
• Acute flares of gouty arthritis may occur infrequently, but over time the interval between attacks may shorten if appropriate measures to correct hyperuricemia are not undertaken.
• Later in the disease, tophaceous deposits of monosodium urate crystals in the skin or subcutaneous tissues may be found.
• These tophi can be anywhere but are often found on the hands, wrists, elbows, or knees.
• It is estimated to take 10 or more years for tophi to develop.
Diagnostic Evaluation of Gout
• A definitive diagnosis of gout requires aspiration of synovial fluid from the affected joint and identification of intracellular crystals of monosodium urate monohydrate in synovial fluid leukocytes.
• Identification of monosodium urate crystals is highly dependent on the experience of the observer.
• Crystals are needle shaped, and when examined under polarizing light microscopy, they are strongly negatively birefringent.
• Crystals can be observed in synovial fluid during asymptomatic periods.
• If an affected joint is tapped, the resulting synovial fluid may have white cells and appear purulent. Such
findings should always raise the question of infection.
• If any clinical features of infection are present, such as high fever, elevated white blood cell count, multiple joints affected, or an identified source of infection, proper diagnosis and treatment are critical.
• Patients with gout can have septic arthritis. Diabetes, alcohol abuse, and advanced age increase the likelihood of septic arthritis.
• In lieu of obtaining a synovial fluid sample from an affected joint to inspect for urate crystals, the clinical
triad of inflammatory monoarthritis, elevated serum uric acid level, and response to colchicine can be used to diagnose gout.
• This approach has limitations, including a failure to recognize atypical gout presentations and the fact that serum uric acid levels can be normal or even low during an acute gout attack.
• In addition, use of colchicine as a diagnostic tool for gout is limited by lack of sensitivity and specificity for
the disease.
• Other conditions such as psoriatic arthritis, sarcoidosis, and Mediterranean fever can respond to colchicine therapy.
• For patients with long-standing gout, radiographs may show punched-out marginal erosions and secondary osteoarthritic changes; however, in an acute first attack radiographs will be unremarkable.
• The presence of chondrocalcinosis on radiographs may indicate pseudogout.
• Some studies have recently examined the use of magnetic resonance imaging and computed tomography to obtain images for patients with gout; however, this is not currently considered part of
normal practice.
URIC ACID NEPHROLITHIASIS
• Clinicians should be suspicious of hyperuricemic states for patients who present with kidney stones, as
nephrolithiasis occurs in 10% to 25% of patients with gout.
• The frequency of urolithiasis depends on serum uric acid concentrations, acidity of the urine, and urinary
uric acid concentration.
• Typically, patients with uric acid nephrolithiasis have a urinary pH of less than 6.0.
• Uric acid has a negative logarithm of the acid ionization constant of 5.5.
• Therefore, when the urine is acidic, uric acid exists primarily in the unionized, less soluble form.
• At a urine pH of 5.0, urine is saturated at a uric acid level of 15 mg/ dL (0.89 mmol/L).
• When the urine pH is 7.0, the solubility of uric acid in urine is increased to 200 mg/dL (11.9 mmol/L).
• For patients with uric acid nephrolithiasis, urinary pH typically is less than 6.0 and frequently less than 5.5.
• When acidic urine is saturated with uric acid, spontaneous precipitation of stones may occur.
• Other factors that predispose individuals to uric acid nephrolithiasis include excessive urinary excretion of
uric acid and highly concentrated urine.
• The risk of renal calculi approaches
50% in individuals whose renal excretion of uric acid exceeds 1,100 mg/ day (6.5 mmol/day).
• In addition to pure uric acid stones, hyperuricosuric individuals are at increased risk for mixed uric acid–calcium oxalate stones and pure calcium oxalate stones.
• Uric acid stones are usually small, round, and radiolucent.
• Uric acid stones containing calcium are radiopaque.
GOUTY NEPHROPATHY
• There are two types of gouty nephropathy: acute uric acid nephropathy and chronic urate nephropathy.
• In acute uric acid nephropathy, acute renal failure occurs as a result of blockage of urine flow secondary to massive precipitation of uric acid crystals in the collecting ducts and ureters.
• This syndrome is a well-recognized complication for patients with myeloproliferative or lymphoproliferative
disorders and is a result of massive malignant cell turnover, particularly after initiation of chemotherapy.
• Chronic urate nephropathy is caused by the long-term deposition of urate crystals in the renal parenchyma.
• Microtophi may form, with a surrounding giant-cell inflammatory reaction.
• A decrease in the kidneys’ ability to concentrate urine and the presence of proteinuria may be the earliest
pathophysiologic disturbances.
• Hypertension and nephrosclerosis are common associated findings.
• Although renal failure occurs in a higher percentage of gouty patients than expected, it is not clear if hyperuricemia per se has a harmful effect on the kidneys.
• The chronic renal impairment seen in individuals with gout may result largely from the coexistence of hypertension, diabetes mellitus, and atherosclerosis.
TOPHACEOUS GOUT
• Tophi (urate deposits) are uncommon in the general population of gouty subjects and are a late complication of hyperuricemia.
• The most common sites of tophaceous deposits for patients with recurrent acute gouty arthritis are the base of the great toe, helix of the ear, olecranon bursae, Achilles tendon, knees, wrists, and hands
• Eventually, even the hips, shoulders, and spine may be affected.
• In addition to causing obvious deformities, tophi may damage surrounding soft tissue, cause joint destruction and pain, and even lead to nerve compression syndromes including carpal tunnel syndrome.
Summary
• Gout is different from hyperuricemia
ACUTE GOUTY ARTHRITIS
• A classic acute attack of gouty arthritis is characterized by rapid and localized onset of excruciating pain, swelling, and inflammation
URIC ACID NEPHROLITHIASIS
The frequency of urolithiasis depends on serum uric acid concentrations, acidity of the urine, and urinary uric acid concentration
TOPHACEOUS GOUT
• Tophi (urate deposits) are uncommon in the general population of gouty subjects and are a late complication of hyperuricemia
Also, Visit:
B. Pharma Notes | B. Pharma Notes | Study material Bachelor of Pharmacy pdf