Alcoholic Liver Disease

Objectives
At the end of this session, student will be able to –
• Explain the Pathogenesis of Alcoholic Liver Disease
• Describe the Symptoms of Alcoholic Liver Disease
• Explain various laboratory diagnosis test for Alcoholic liver Disease
Alcoholic Liver Disease
Alcoholic liver disease is the term used to describe the spectrum of liver injury associated with acute and chronic alcoholism
Signs and Symptoms
• Progresses in the liver as inflammation (hepatitis) and leads to fatty liver and cirrhosis
Early Symptoms
- Fatigue: Feeling excessively tired is one of the initial signs of ALD.
- Abdominal Discomfort: A vague, persistent pain or discomfort in the abdominal area.
- Loss of Appetite: Reduced interest in food and subsequent weight loss.
- Nausea and Vomiting: Frequent feelings of nausea and occasional vomiting.
- Jaundice: A yellowing of the skin and whites of the eyes.
Advanced Symptoms
- Ascites: Accumulation of fluid in the abdominal cavity.
- Portal Hypertension: High blood pressure in the portal vein.
- Confusion and Impaired Cognitive Function: Due to the liver’s inability to filter toxins.
- Easy Bruising and Bleeding: A decline in platelet production.
- Swelling in the Legs and Ankles: Known as edema.
Risk factors
• Occurs after many years of excessive drinking
• Acute alcoholic hepatitis – Binge drinking
• Severe drinking – Life threatening
• Genetic factors – Women have increased susceptibility to develop advanced alcoholic liver disease with much lesser alcohol intake
• Malnutrition
• Toxicity of ethanol in liver
• Infection – Hepatitis C infection
Distinctive forms of Alcoholic Liver Disease
Hepatic Steatosis (Fatty liver)
• Moderate consumption – Deposition of small lipid droplets in hepatocytes
• Excessive consumption – accumulation of lipids in macrovascular droplets
• Nucleus gets displaced, Enlarged liver
Alcoholic hepatitis
• Necrosis of liver cells in centrilobular region
• Neutrophillic reaction
• Fibrosis
Alcoholic Cirrhosis
• Irreversible – Final stage
• Liver turns brown, shrunken and non-fatty appearance
• Resembles post necrotic cirrhosis
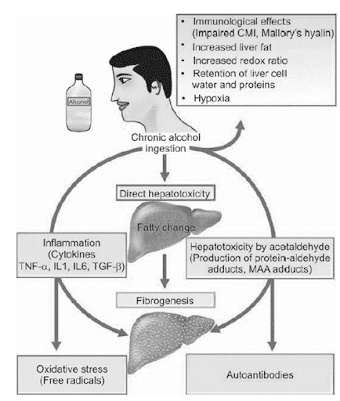
Pathogenesis of Alcoholic Liver Disease
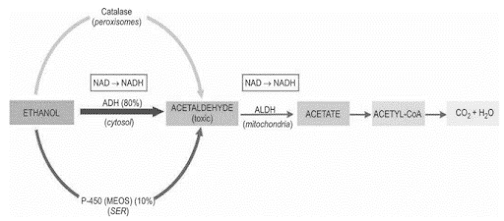
Ethanol Metabolism
ADH = Alcohol Dehydrogenase; ALDH or ACDH = Hepatic Acetaldehyde Dehydrogenase; NAD = Nicotinamide Adenine Dinucleotide; NADH = Reduced NAD
• Direct hepatotoxicity by ethanol to microtubules, mitochondria, membrane hepatocytes
• Hepatotoxicity by ethanol metabolites
– Production of protein-aldehyde adducts
– Formation of malo-di-aldehyde-acetaldehyde (MAA)
• Oxidative Stress – oxidation of ethanol by cytochrome 450 oxidase, generation of free radicals and oxidative damage
• Immunological attacks on hepatocytes
• Fibrogenesis
– Damaged hepatocytes,
– Malon-di-aldehyde-acetaldehyde adducts,
– Activated kupffer cells, and
– Direct stimulation by acetaldehyde
Laboratory Diagnosis For Alcoholic Liver Disease
Diagnosing ALD involves a combination of clinical evaluation, laboratory tests, and imaging techniques.
Blood Tests
- Liver Function Tests: Assess liver enzymes and bilirubin levels.
- Complete Blood Count: Detect changes in blood cells.
- Carbohydrate-Deficient Transferrin (CDT): A specific marker of heavy alcohol use.
Imaging Techniques
- Ultrasound: Used to evaluate liver size and detect abnormalities.
- CT Scan: Provides detailed images of the liver’s structure.
- FibroScan: Measures liver stiffness, a sign of fibrosis.
• Elevated transaminases: increase in SGOT (AST) is more than that of SGPT (ALT)
• Rise in serum γ-glutamyl transpeptidase (γ-GT)
• Elevation in Serum alkaline phosphatase
• Hyperbilirubinaemia
• Hypoproteinaemia with reversal of albumin-globulin ratio
• Prolonged prothrombin time and partial thromboplastin time
• Anemia and Neutrophilic leucocytosis
Preventive Measures
Preventing ALD begins with responsible alcohol consumption.
Reducing Alcohol Consumption
- Limit alcohol intake to recommended guidelines.
- Seek professional help if struggling with alcohol dependence.
Maintaining a Healthy Lifestyle
- Eat a balanced diet.
- Exercise regularly.
- Ensure regular check-ups with your healthcare provider.
Treatment Options
When diagnosed with ALD, it’s crucial to take appropriate steps.
Lifestyle Changes
- Alcohol Abstinence: The most effective treatment.
- Nutritional Support: Ensure proper nutrient intake.
Medications
- Corticosteroids: May be prescribed for severe cases.
- Ursodeoxycholic Acid (UDCA): Used to manage cholestasis.
Conclusion
Alcoholic Liver Disease is a serious condition that can have devastating consequences. Understanding its symptoms, pathogenesis, and diagnostic methods is essential for early detection and effective management. Responsible alcohol consumption and a healthy lifestyle are key to prevention. In case of diagnosis, prompt intervention is crucial for a better prognosis.
FAQs on Alcoholic Liver Disease
1. Can occasional alcohol consumption lead to ALD?
Occasional alcohol consumption is less likely to lead to ALD. However, it’s essential to be mindful of your alcohol intake, as the risk accumulates over time.
2. Is ALD reversible?
In the early stages, ALD is reversible by abstaining from alcohol and making lifestyle changes. Advanced stages may have irreversible damage.
3. Are there any specific diets for ALD patients?
A well-balanced diet is recommended for ALD patients, with a focus on limiting sodium and ensuring adequate protein intake.
4. How is ALD different from non-alcoholic fatty liver disease (NAFLD)?
ALD is caused by excessive alcohol consumption, while NAFLD is linked to obesity and metabolic factors. They have different underlying causes.
5. What are the long-term complications of ALD if left untreated?
If left untreated, ALD can progress to cirrhosis, liver failure, and an increased risk of liver cancer, which can be life-threatening.
Summary
• Alcohol liver disease is damage to liver and its function due to alcohol abuse
• Progresses in the liver as inflammation (hepatitis) and leads to fatty liver and cirrhosis
• Major forms include hepatic steatosis, hepatitis, cirrhosis
• Alcohol is a caloric food source which displaces nutrients
• Causes the activation of Kupffer cells and release of proinflammatory mediators

1 thought on “Alcoholic Liver Disease – B. Pharma 2nd Semester Pathophysiology notes pdf”
Comments are closed.