Anaemia

Objective
At the end of this PDF Notes, students able to
• Explain the etiology of iron deficiency anaemia
• Elaborate the pathogenesis of iron deficiency anaemia and its treatment
BLOOD
• Components of Blood
Anemia
• Condition in which the oxygen-carrying capacity of blood is reduced
• Characterized by reduced numbers of RBCs or a decreased amount of hemoglobin in the blood
General manifestations of anemia
Reduced oxygen delivery can result in the following:
• Ischemia
• Fatigability
• Breathlessness upon exertion
• Exercise intolerance
• Pallor
• Increased susceptibility to infection
Classification of Anemia
1) Based on Size changes
2) Color changes (due to altered hemoglobin content)
• Normochromic — Normal hemoglobin concentration
• Hypochromic — Reduced hemoglobin concentration
Example: Iron deficiency anemia may be classified as a microcytic, hypochromic anemia as both red blood cell size and hemoglobin content are reduced
3) Blood loss anemia: Anemia that results from acute blood loss.
4) Iron-deficiency anemia: It can occur as a result of iron-deficient diets
5) Cobalamin-deficiency or folate-deficiency anemia
6) Inherited anemia- Sickle cell anaemia
Iron Deficiency Anemia
• The commonest nutritional deficiency disorder present throughout the world is iron deficiency
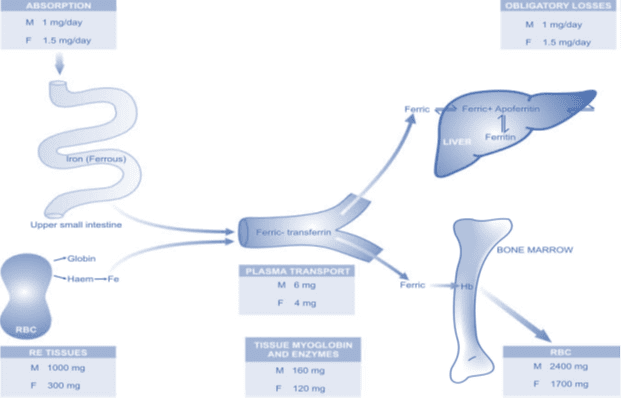
Absorption
• Haem iron is better in absorption than non haem iron
• Non-haem iron is released as ferrous or ferric form
• Transport across the membrane by divalent metal transporter 1 (DMT 1)
TRANSPORT:
• Iron is transported in plasma bound to a β-globulin, transferrin, synthesised in the liver
• Transferrin bound iron utilise for haemoglobin synthesis.
• Transferrin is reutilised after iron is released from it.
EXCRETION:
The body is unable to regulate its iron
content by excretion alone. The amount of iron lost per day is 0.5-1 mg.
DISTRIBUTION. In an adult, iron is distributed in the body as under:
• 1. Haemoglobin—(65%).
• 2. Myoglobin—(3.5%).
• 3. Haem and non-haem enzymes—(0.5%).
• 4. Transferrin-bound iron—(0.5%)
• 5. Ferritin and haemosiderin—a (30%).
Iron absorption
Absorption of Iron
Pathogenesis of Iron deficiency anaemia
• Iron deficiency anaemia develops when the supply of iron is inadequate for the requirement of haemoglobin synthesis.
• The development of iron deficiency depends upon one or more of the following factors:
Etiology of Iron deficiency anaemia
I. INCREASED BLOOD LOSS
1. Uterine e.g. excessive menstruation in reproductive years, repeated miscarriages, at onset of menarche, post-menopausal uterine bleeding
2. Gastrointestinal e.g. peptic ulcer, haemorrhoids, hookworm infestation, cancer of stomach and large bowel, oesophageal varices, hiatus hernia, chronic aspirin ingestion, ulcerative colitis, diverticulosis
3. Renal tract e.g. haematuria, haemoglobinuria
4. Nose e.g. repeated epistaxis
5. Lungs e.g. haemoptysis
II. INCREASED REQUIREMENTS
1. Spurts of growth in infancy, childhood and adolescence
2. Prematurity
3. Pregnancy and lactation
III. INADEQUATE DIETARY INTAKE
1. Poor economic status
2. Anorexia e.g. in pregnancy
3. Elderly individuals due to poor dentition, apathy and financial constraints
IV. DECREASED ABSORPTION
1. Partial or total gastrectomy
2. Achlorhydria
3. Intestinal malabsorption such as in coeliac disease
Clinical Features of Iron deficiency anaemia
• Iron deficiency anaemia is much more common in women between the age of 20 and 45 years than in men
• More frequent in premature infants.
Clinical consequences of iron deficiency:
1) anemia
2) epithelial tissue changes
Treatment of Iron deficiency anaemia
The treatment of iron deficiency anemia typically involves addressing the underlying cause and replenishing iron levels. It may include:
- Dietary Changes: Increasing the intake of iron-rich foods, including red meat, dark leafy greens, beans, and iron-fortified cereals.
- Iron Supplements: If dietary changes are insufficient, iron supplements may be prescribed by a healthcare provider.
- Management of Underlying Conditions: Treating any gastrointestinal disorders or chronic bleeding issues that contribute to the anemia.
- Blood Transfusions:In severe cases, where hemoglobin levels are critically low, a blood transfusion may be necessary.
The management of iron deficiency anaemia consists of 2 essential principles:
1) Correction of disorder causing the anaemia: checkup and investigations.
2) Correction of iron deficiency:
i) Oral therapy ii) Parenteral therapy
Frequently Asked Questions (FAQ)
Q1: Can iron deficiency anemia be prevented? A1: Yes, it can often be prevented by maintaining a diet rich in iron and promptly addressing any underlying conditions that may lead to anemia.
Q2: What are the symptoms of iron deficiency anemia? A2: Common symptoms include fatigue, weakness, pale skin, shortness of breath, cold extremities, and brittle nails.
Q3: Is iron deficiency anemia more common in certain demographics? A3: Yes, it is more prevalent in women of childbearing age, pregnant women, and individuals with specific medical conditions.
Q4: How is iron deficiency anemia diagnosed? A4: Diagnosis typically involves blood tests to measure hemoglobin and serum ferritin levels, assessing iron stores in the body.
Q5: Are there potential complications of untreated iron deficiency anemia? A5: Yes, untreated anemia can lead to more severe health problems, including heart issues and cognitive impairment.
Summary
• Anaemia is the condition in which the oxygen-carrying capacity of blood is reduced
• Characterized by reduced numbers of RBCs or a decreased amount of hemoglobin in the blood
• The commonest nutritional deficiency disorder present throughout the world is iron deficiency
• Iron deficiency anaemia develops when the supply of iron is inadequate for the requirement of haemoglobin synthesis








Comments are closed.