GOUT
Objective
At the end of this lecture, student will be able to
- Define gout
- Explain the epidemiology of gout
- Describe the etiology of gout
- Explain pathophysiology of gout
GOUT
• The term gout describes a heterogeneous clinical spectrum of diseases including hyperuricemia, recurrent attacks of acute arthritis associated with monosodium urate crystals in synovial fluid leukocytes, deposits of monosodium urate crystals (tophi) in tissues in and around joints, interstitial renal disease, and uric acid nephrolithiasis.
• The underlying metabolic disorder of gout is hyperuricemia, defined physiochemically as serum that is supersaturated with monosodium urate.
Gout Symptoms
The hallmark symptom of gout is intense joint pain, typically affecting the big toe, although it can also occur in other joints. Other symptoms may include swelling, redness, and warmth in the affected area. Gout attacks can come on suddenly and be extremely painful, often waking individuals from sleep.
Epidemiology of Gout
• There is a direct correlation between serum uric acid concentration and both the incidence and prevalence of gout.
• Population studies have shown that serum urate concentration correlates with increasing age, serum creatinine, blood urea nitrogen, male gender, blood pressure, body weight, and alcohol intake.
• The incidence of gout -higher for individuals -higher amounts of meat or fish.
• Gout affects men about seven to nine times more often than women.
• The incidence of gout increases with age, peaking at 30 to 50 years of age, with an annual incidence ranging from 1 in 1,000 for men ages 40 to 44 years and 1.8 in 1,000 for those ages 55 to 64 years.
• The lowest rates of gout are observed in young women, approximately 0.8 cases per 10,000 patient-years.
• Serum uric acid levels in women approach those of men once menopause has occurred
• Gout in men younger than 30 years of age or in premenopausal women may indicate an inherited enzyme defect or the presence of renal disease
Etiology and Pathophysiology of Gout
• In humans, the production of uric acid is the terminal step in the degradation of purines.
• Normal uric acid levels are near the limits of urate solubility, because of the delicate balance that exists between the amount of urate produced and excreted.
• Humans have higher uric acid levels than other mammals because they do not express the enzyme uricase, which converts uric acid to the more soluble allantoin.
• Gout occurs exclusively in humans in whom a miscible pool of uric acid exists
• Under normal conditions, the amount of accumulated uric acid is about 1,200 mg in men and about 600 mg in women
• The size of the urate pool is increased several fold in individuals with gout.
• This excess accumulation may result from either overproduction or underexcretion of uric acid
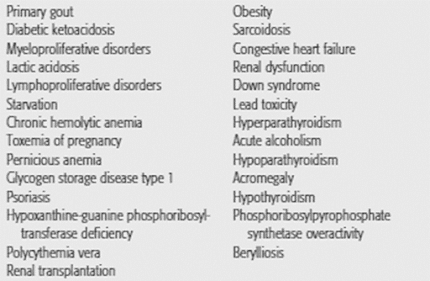
• Several conditions are associated with either decreased renal clearance or an overproduction of uric acid, leading to hyperuricemia
OVERPRODUCTION OF URIC ACID
• The purines from which uric acid is produced originate from three sources:
– Dietary purine
– Conversion of tissue nucleic acid to purine nucleotides
– De novo synthesis of purine bases
• The purines derived from these three sources enter a common metabolic pathway leading to the production of either nucleic acid or uric acid
• Under normal circumstances, uric acid may accumulate excessively if production exceeds excretion
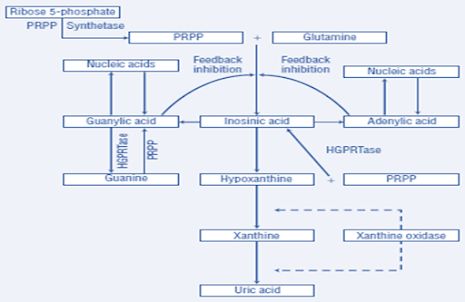
Purine metabolism
• The average human produces about 600 to 800 mg of uric acid each day.
• Dietary purines play an unimportant role in the generation of hyperuricemia in the absence of some derangement in purine metabolism or elimination.
• Diet modifications are important for patients with such problems who develop symptomatic hyperuricemia.
• Several enzyme systems regulate purine metabolism.
Conditions Associated with Hyperuricemia
• Abnormalities in these regulatory systems can result in overproduction of uric acid.
• Uric acid may also be overproduced as
– A consequence of increased breakdown of tissue nucleic acids
– Excessive rates of cell turnover
– Myeloproliferative and lymphoproliferative disorders
– Polycythemia vera
– Psoriasis
– Some types of anemias
• Cytotoxic medications used to treat these disorders can result in overproduction of uric acid secondary to lysis and breakdown of cellular matter.
• Two enzyme abnormalities resulting in an overproduction of uric acid have been well described
• The first is an increase in the activity of phosphoribosyl pyrophosphate (PRPP) synthetase, which leads to an increased concentration of PRPP
• PRPP is a key determinant of purine synthesis and uric acid production
• The second is a deficiency of hypoxanthine-guanine phosphoribosyltransferase (HGPRT)
• HGPRT is responsible for the conversion of guanine to guanylic acid and hypoxanthine to inosinic acid
• These two conversions require PRPP as the cosubstrate and are important reactions involved in the synthesis of nucleic acids
• A deficiency in the HGPRT enzyme leads to increased metabolism of guanine and hypoxanthine to uric acid and to more PRPP to interact with glutamine in the first step of the purine pathway
• Complete absence of HGPRT results in the childhood Lesch-Nyhan syndrome, characterized by choreoathetosis, spasticity, mental retardation, and markedly excessive production of uric acid
• A partial deficiency of the enzyme may be responsible for marked hyperuricemia in otherwise normal, healthy individuals
UNDEREXCRETION OF URIC ACID
• Normally, uric acid does not accumulate as long as production is balanced with elimination
• About two thirds of the daily uric acid production is excreted in the urine and the remainder is eliminated through the gastrointestinal tract after enzymatic degradation by colonic bacteria
• The vast majority of patients (80% to 90%) with gout have a relative decrease in the renal excretion of uric acid for an unknown reason (primary idiopathic hyperuricemia)
• A decline in the urinary excretion of uric acid to a level below the rate of production leads to hyperuricemia and an increased miscible pool of sodium urate
• Almost all the urate in plasma is freely filtered across the glomerulus
• The concentration of uric acid appearing in the urine is determined by multiple renal tubular transport processes in addition to the filtered load.
• Evidence favors a four-component model including glomerular filtration, tubular reabsorption, tubular secretion, and postsecretory reabsorption
• Approximately 90% of filtered uric acid is reabsorbed in the proximal tubule, probably by both active and passive transport mechanisms
• There is a close linkage between proximal tubular sodium reabsorption and uric acid reabsorption
• A conditions that enhance sodium reabsorption (e.g., dehydration) also lead to increased uric acid reabsorption
• The exact site of tubular secretion of uric acid has not been determined; this too appears to involve an active transport process.
• Postsecretory reabsorption occurs somewhere distal to the secretory site.
• By enhancing renal urate reabsorption, insulin resistance is also associated with gout.
• The pathophysiologic approach to the evaluation of hyperuricemia requires determining whether the patient is overproducing or underexcreting uric acid
• This can be accomplished by placing the patient on a purine-free diet for 3 to 5 days and then measuring the amount of uric acid excreted in the urine in 24 hours
• As it is very difficult to maintain a purine-free diet for several days, this test is done infrequently in clinical practice
• Nevertheless, when it is performed, individuals who excrete more than 600 mg on a purine-free diet may be considered overproducers
• Nevertheless, when it is performed, individuals who excrete more than 600 mg on a purine-free diet may be considered overproducers
SUMMARY
• Prevalence is greater in men (5.9%; 6.1 million) than women (2.0%; 2.2 million)
• Caused by the deposition of monosodium urate crystals in tissues
• Uric acid is a metabolic by-product of purine catabolism
FAQs
- Can gout be cured completely? Gout can be managed effectively, but a complete cure is rare.
- What are some natural remedies for gout? Cherry juice, ginger, and herbal supplements are some natural remedies that may help alleviate gout symptoms.
- How can I prevent gout flare-ups? Staying hydrated, avoiding trigger foods, and taking prescribed medications can help prevent gout attacks.
- Can gout affect other joints besides the big toe? Yes, gout can affect other joints, including the ankle, knee, and wrist.
- Is gout hereditary? While genetics can play a role, gout is often influenced by lifestyle and dietary choices.
For Gout PDF Notes Click on Download Button
Also, Visit:
B. Pharma Notes | B. Pharma Notes | Study material Bachelor of Pharmacy pdf

Comments are closed.