Hepatitis
Objectives
At the end of this lecture, students will be able to –
• Identify the symptoms of hepatitis
• Describe the structure of HBV
• Explain different stages of hepatitis
Hepatitis
Hepatitis is a group of viral infections that primarily affect the liver. It can lead to a range of symptoms and health complications. In this article, we will explore the symptoms of hepatitis, describe the structure of the Hepatitis B virus (HBV), and explain the different stages of hepatitis.
• Inflammation of liver
• Results in damage to hepatocytes with subsequent cell death
Etiology of hepatitis
• Viral infections – Hepatitis A, B, C, D, E ; Epstein barr virus, yellow fever virus, cytomegalo virus & herpes virus
• Autoimmune chronic hepatitis
• Toxins, Alcohol
• Drugs used for the treatment of tuberculosis e.g. Isoniazid
Symptoms of hepatitis
| Initial symptoms | Final symptoms |
| Hepatic symptoms are flu like | Jaundice |
| Mild fever, Chills | Dark urine |
| Headache | Pale faeces containing puss cells |
| Nausea, Vomiting, Diarrhoea | Pruritis |
| Anorexia, Fatigue | Enlargement of spleen |
| Slight abdominal pain | Urticaria |
| Aching of joints | Dizziness, Drausiness, circulation problem |
Types of hepatic viruses
| Name of virus | Content | Mode of spread |
| Hepatitis A virus (HAV) | RNA | Faeces |
| Hepatitis B virus (HBV) | DNA | Parenteral, Sexual contact, Blood transfusion, Babies born to HBV infected mothers |
| Hepatitis C virus (HCV) | RNA | Parenteral transmission, IV drug abuse, needle sharing |
| Hepatitis D virus (HDV) | RNA | Super infection |
| Hepatitis E virus (HEV) | RNA | Transmitted enterically |
| Hepatits G virus (HGV) | RNA | Parenterally transmitted hepatotropic virus |
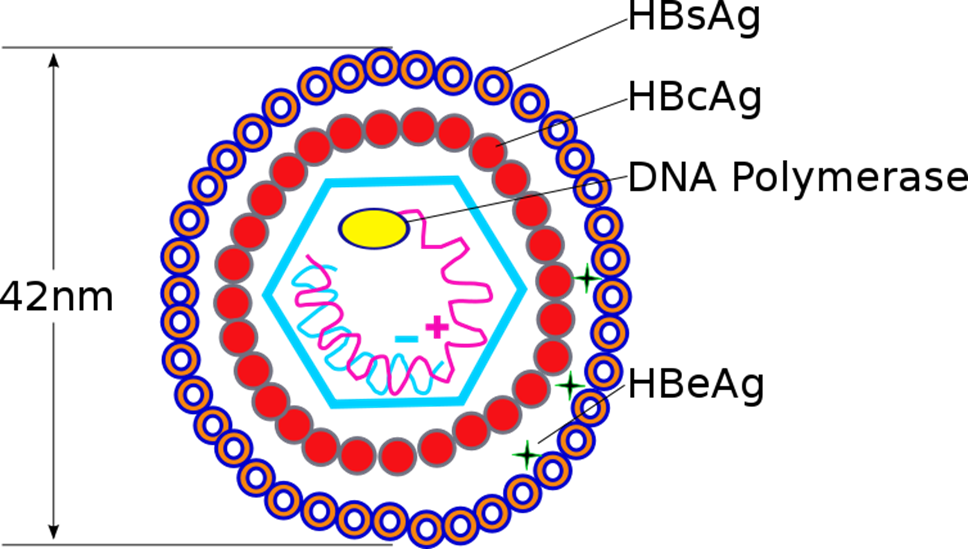
Structure of HBV
The Hepatitis B virus (HBV) is a member of the Hepadnaviridae family. Its structure consists of several key components:
- Outer Envelope: The virus has an outer envelope derived from the host cell’s membrane. This envelope contains proteins that are essential for the virus’s ability to infect liver cells.
- Core Capsid: Inside the envelope, HBV has a core capsid that contains the viral DNA. This core is made up of protein subunits and plays a crucial role in the virus’s replication.
- DNA: The genetic material of HBV is circular, partially double-stranded DNA. This DNA serves as the template for viral replication.
• Only DNA containing virus
• Belongs to group ‘hepadnaviridae’
• Diameter- 42 nm; incubation period is 6-8 weeks
• Comprises of core and a capsule
• Core consists of DNA & DNA polymerase
• Core is surrounded by markers
– Hepatitis B core antigen (HBc Ag)
– Hepatitis B envelope antigen (HBe Ag)
– Hepatitis B surface antigen (HBs Ag)
Mode of transmission of Hepatitis
• Present in all body secretion
• A close contact with an infected person spreads the disease
• By blood transfusion
• Not through fecal matter
Stages of hepatitis (Assessed by different markers)
Stage 1
• HBs Ag is identified in asymptomatic phase
• It appears even before the onset of a disease
• Reaches the peak level during disease stage
• The counts become less with in 3-6 months
Stage 2
• HBe Ag, HBV DNA, DNA polymerase appears
• HBe Ag – indicates the progression of infection
• Continues viral replication
Stage 3
• IgM and anti HBc is detected
• Ab is identified just before the onset of symptoms
• After several months of infections IgG and anti HBc
Phases of HBV infection
Proliferative phase
• Shows the presence of symptoms
• DNA of HBV has accessory replicative chromosomes and forms virions
• HBs antigen binds with MHC class molecule and activated CD8+ T-cells
Integrative phase
• Viral DNA gets incorporated into the host genome
• Damage of hepatocytes by activation of CD8+ T- cells
Types of Hepatitis
Acute hepatitis
comprises of 4 phases
1. Incubation period –depends on type of virus
• HAV – 12 weeks
• HBV – 10 weeks
• HCV – 7 weeks
• HDV – 6 weeks
• HEV – 2-8 weeks
Patient does not show any signs or symptoms in incubation period
2. Symptomatic pre – icteric phase
• Non specific symptoms like fatigue, nausea, vomiting, weight loss, low fever, headache, muscle & joint aches, diarrhoea
3. Symptomatic icteric phase
• Yellow coloration appears
• Jaundice appears in 3rd stage
4. Phase of recovery
• Takes place depending upon the severity of infection
Chronic hepatitis
• Hepatic diseases remain for more than 6 months
• Inflammation & necrosis takes place
• Fatigue, Malaise, Lack of apetite, mild jaundice
• Symptoms are highly variable & not predictive in nature
Cirrhosis:
In some cases, chronic hepatitis can progress to cirrhosis, which is characterized by extensive scarring of the liver tissue. Cirrhosis can lead to severe liver dysfunction.
Liver Cancer:
Individuals with long-standing, untreated chronic hepatitis, particularly Hepatitis B and C, are at an increased risk of developing liver cancer.
Fulminant Hepatitis:
In some rare cases, acute hepatitis can progress to fulminant hepatitis, a severe and life-threatening form of the disease. This stage is characterized by rapid liver failure and requires immediate medical intervention, often with a liver transplant.
Asymptomatic Carrier State:
Some individuals, particularly those with chronic Hepatitis B or C, may become carriers of the virus without exhibiting noticeable symptoms. These carriers can still transmit the virus to others, and monitoring their condition is essential.
Resolution:
In a fortunate scenario, acute hepatitis can resolve on its own, with the body successfully clearing the virus. This typically occurs with Hepatitis A but can also happen with other forms. Individuals who recover from acute hepatitis usually develop immunity to that specific strain of the virus.
Management of Hepatitis
- Medical Evaluation: If you suspect you have hepatitis or exhibit symptoms, it’s crucial to seek medical evaluation. Your healthcare provider will conduct blood tests to determine the type of hepatitis and its stage.
- Antiviral Medications: In the case of chronic hepatitis, particularly Hepatitis B and C, antiviral medications may be prescribed to slow down viral replication and reduce liver inflammation.
- Supportive Care: Proper rest, hydration, and a balanced diet can help your body recover from acute hepatitis. Avoid alcohol and any medications that can harm the liver.
- Vaccination: For Hepatitis B, vaccination is available and highly effective for prevention. Vaccination is recommended for individuals at risk of exposure to the virus.
- Regular Monitoring: People with chronic hepatitis, especially those with advanced liver disease, require regular monitoring to assess the progression of the condition and evaluate the need for additional treatment or liver transplantation.
- Prevention: Prevention is key to avoiding hepatitis. Practicing safe sex, using clean needles, avoiding sharing personal items that may have blood on them, and maintaining good hygiene are essential preventive measures.
- Liver Transplant: In severe cases of liver damage or cirrhosis, a liver transplant may be necessary to replace the damaged liver with a healthy one.
Summary
• Hepatitis is inflammation of liver that results in damage to hepatocytes with subsequent cell death
• It may occur due to viral , autoimmune chronic hepatitis, Toxins, Alcohol and drugs
• HBV is main causative organism
• Types of hepatitis include acute and chronic