Hypertension
Objective
At the end of this PDF, student will be able to
• Define hypertension
• Classify various types of hypertension
• Explain the pathogenesis involved in the development of hypertension
• Describe the complications associated with the development of hypertension
Hypertension
Hypertension, often referred to as high blood pressure, is a chronic medical condition where the force of blood against the artery walls is consistently too high. This condition can lead to severe health problems if left unmanaged.
Persistently elevated arterial blood pressure [BP]
Associated with both functional and morphologic alteration of blood vessels
• Arterial BP – generated by the interplay between blood flow and the resistance to blood flow
• Measured in mmHg
2 types of arterial blood pressure
• Systolic BP (SBP)- achieved during cardiac contraction
• Diastolic BP (DBP)- achieved after contraction when the cardiac chambers are filling
SBP – DBP = pulse pressure (measure of arterial wall tension)
― Cardiac output – major determinant of SBP
― Total peripheral resistance determines DBP
• Mean arterial pressure [MAP] – Average pressure throughout the cardiac cycle of contraction
• During cardiac cycle 2/3rd time spent in diastole and 1/3rd time in systole
MAP= [SBP (1/3)] +[DBP (2/3)]
BP= Cardiac output × Total peripheral
resistance
Clinical classification of hypertension
| Category | Systolic (mm Hg) | Diastolic (mm Hg) |
| Normal | < 130 | <85 |
| High normal | 130-139 | 85-89 |
| Hypertension | ||
• Mild (Stage 1) | 140-159 | 90-99 |
• Moderate (Stage 2) | 160-179 | 100-109 |
• Severe (Stage 3) | 180-209 | 110-119 |
• Very severe (Stage 4) | ≥ 210 | ≥ 120 |
| Malignant hypertension | > 200 | ≥ 140 |
Etiological classification of hypertension
A. Primary essential hypertension
• Genetic factors
• Racial and environmental factors
• Risk factors modifying the course of HT
B. Secondary hypertension
• Renal – Renovascular
Renal parenchymal disease
• Endocrine – Adrenocortical hyperfunction
Hyperparathyroidism
Oral contraceptives
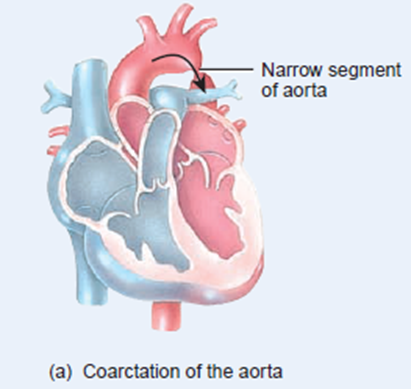
• Coarctation of aorta
• Neurogenic
Clinical classification of primary and secondary hypertension
Benign hypertension
• Observed in 95% of patients
• Slow rise in BP taking years to develop
Malignant/ accelerated hypertension
• Observed in 5-10% of patients
• Rapid rise in BP to 200/140 mm Hg or more
• If left untreated, patient’s life expectancy decreases
Symptoms of Hypertension
When BP is severe, following symptoms are observed
• Nose bleeding
• Irregular heart beat
• Head ache
• Dizziness
• Fatigue
• Flushed face
• Breathing difficulties
• Strong tendency to uinate
• Vertigo, tinnitus, etc.,
Malignant hypertension is characterized by
• Pulsating headache beneath the eye
• Visual disturbance
• Nausea and vomiting
• Disturbed sleep
Pathogenesis of Hypertension
BP is the product of
• Cardiac output
• Total peripheral vascular resistance
- Cardiac output
– Volume of blood that circulates through systemic blood vessels each minute
– Dependent on stroke volume (SV)
– SV – Volume of blood ejected by the left ventricle during each contraction
- Peripheral resistance depends on
̶ Viscosity of blood
̶ Diameter of the blood vessel
̶ Compliance
• High viscosity – high pressure to pass through vascular bed
• High pressure to pass through constricted and non-complaint blood vessels
BP is controlled by
- Neural component
- Peripheral auto regulatory mechanism
- Humoral mechanism
- Vascular endothelial mechanism
Neural component
• Both CNS & ANS controls BP
Centers in CNS are
̶ Vasomotor center in Medulla
̶ Vagal nucleus
̶ Area postrema
̶ Nuclues tractus solitarii
̶ Maintenance of BP by sympathetic nervous system through α and β adrenergic receptors
++ post synaptic α1 receptors ―vasoconstriction ― ↑ BP
++ pre synaptic α2 receptors ― negative feedback on NA release
++ β1 in heart ― ↑ HR and contractility
++ β2 in arterioles and venules ― vasodilation
Change in BP senses by barro receptors in carotid artery and aortic arch
• Respond to change in arterial pressure
• Transmitted to brain through IX cranial nerve and vagus nerve
• ↑ discharge from barroreceptors − depression of vasomotor center − excitation of nucleus ambiguus − reverts change in BP
Peripheral auto regulatory mechanism
• Normal case – volume and pressure adaptive mechanism of kidney maintains BP
↓ BP – adaptation of kidney ̶ more Na+ and H2O retention
↑BP – adaptation of kidney ̶ Na+ and H2O excretion – ↓ blood volume & cardiac output
Humoral mechanism
- Renin Angiotensin Aldosterone system
- Natriuretic hormone
- Insulin resistance and hyperinsulinemia
Renin-Angiotensin-aldosterone system
Natriuretic hormone
• Inhibits Na+ /K+ ATP ase
• Interferes with Na+ transport across cell membrane
• ↑ Na+ in body fluids – ↑ Natriuretic hormone – ↑ urinary excretion of Na+ and H2O
• Blocks active transport of Na+ out of the walls of arterioles – ↑ vascular tone and BP
Insulin resistance and hyper insulinemia
• Causes Na+ retention
• Increases sympathetic activity
• Increases vascular resistance
• Increases BP
Vascular endothelial mechanism
• Regulates blood vessel tone
• Vasodilating substances – Nitric oxide, Prostacyclin (PI2) and bradykinin – Hypotension
• Vasoconstrictors – Angiotensin II and Endothelin I – ↑BP
Effect of dietary Na+ Ca2+ K+ on BP
• ↑ intra cellular Ca2+ – alters smooth muscle function on blood vessels – ↑ Peripheral vascular resistance
• K+ depletion – ↑ Peripheral vascular resistance
• ↑ Na+ in body fluids & in arterial wall – ↑ BP
Complications of Hypertension
• Blood vessels
– Large arterioles dialatess
– Smaller arterioles get damaged
• Eye – Arterial narrowing, haemmorhage
• Heart – Hypertropy of left ventricles, heart failure
• Kidney – Nephrosclerosis, renal damage, death in uremia
• Brain – Rupture of damaged blood vessels, encephalopathy, cerebral edema
Summary
• Persistently elevated arterial blood pressure is called hypertension
• Hypertension can be classified as benign or malignant or accelerated hypertension
• HT can also be classifies as primary and secondary HT based on etiology
• BP is controlled by neuronal component, humoral mechanism, peripheral autoregultory mechanism and vascular endothelial mechanism
• Any defects in the functioning of these mechanisms leads to the development of HT
• HT is affects kidneys, blood vessels, brain and predisposed to many cardiovascular diseases
Frequently Asked Questions
- What is the leading cause of hypertension?
- The exact cause of primary hypertension is often unknown, but it’s commonly linked to lifestyle factors, genetics, and age.
- Can hypertension be hereditary?
- Yes, hypertension can run in families, making genetics a significant risk factor.
- What are the long-term complications of uncontrolled hypertension?
- Uncontrolled hypertension can lead to heart disease, stroke, kidney damage, and vision problems.
- How is hypertension diagnosed?
- Hypertension is diagnosed through repeated blood pressure measurements. High readings over time indicate the condition.
- Are there natural ways to manage hypertension without medication?
- Yes, lifestyle modifications such as a heart-healthy diet and regular exercise can help manage hypertension without medication.