Meningitis B Pharma 2nd Semester Pathophysiology notes pdf
Objective
At the end of the class the students will be able to
• Define meningitis
• Difference between pachymeningitis, leptomeningitis
• Discuss the etiology, pathogenesis and clinical Acute Pyogenic Meningitis, Chronic (Tuberculous and Cryptococcal) Meningitis,
Meningitis
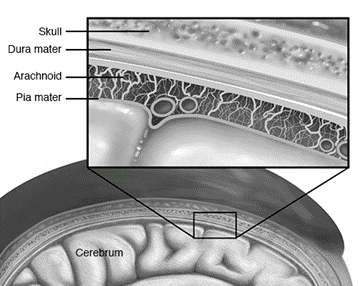
It is inflammatory involvement of the meninges.
• Meningitis may involve the dura called pachymeningitis,
• leptomeninges (pia-arachnoid) termed leptomeningitis
• Pachymeningitis: inflammation from chronic suppurative otitis media or from fracture of the skull.
• Extradural abscess may form by suppuration between the bone and dura- penetrate the dura and form a subdural abscess.
Leptomeningitis, commonly called meningitis- infection
• Infectious meningitis is broadly classified into 3 types:
1. acute pyogenic,
2. acute lymphocytic (viral, aseptic)
3. chronic (bacterial or fungal)
Acute Pyogenic Meningitis
• Acute pyogenic or acute purulent meningitis is acute infection of the pia-arachnoid and of the CSF enclosed in the subarachnoid space.
ETIOPATHOGENESIS-Acute Pyogenic Meningitis
Causative organisms vary with age of the patient
- Escherichia coli
- Haemophilus influenzae
- Neisseria meningitidis
- Streptococcus pneumoniae
• routes of infection as follows:
1. Most commonly by the blood stream.
2. From an adjacent focus of infection.
3. By iatrogenic infection such as introduction of microorganisms at operation or during lumbar puncture.
Symptoms of Meningitis
CLINICAL FEATURES AND DIAGNOSIS of MENINGITIS
Acute bacterial meningitis is a medical emergency.
• The immediate clinical manifestations are fever, severe headache, vomiting, drowsiness, stupor, coma, and occasionally, convulsions
• The diagnosis is confirmed by examining CSF
1. Naked eye appearance of cloudy or frankly purulent CSF.
2. Elevated CSF pressure (above 180 mm water).
3. Polymorphonuclear neutrophilic leucocytosis in CSF(between 10-10,000/μl).
4. Raised CSF protein level (higher than 50 mg/dl).
5. Decreased CSF sugar concentration (lower than 40 mg/dl)
6. Bacteriologic examination by Gram’s stain
Acute Lymphocytic (Viral, Aseptic) Meningitis
• Acute lymphocytic meningitis is a viral or aseptic meningitis, especially common in children and young adults.
• Etiologic agents are numerous viruses such as enteroviruses, mumps, ECHO viruses, coxsackie virus, Epstein-Barr virus, herpes simplex virus-2, arthropode-borne viruses and HIV
• viral meningitis has a benign and self-limiting clinical course of short duration and is invariably followed by complete recovery
Chronic (Tuberculous and Cryptococcal) Meningitis
• There are two principal types of chronic meningitis—bacterial (tuberculous meningitis) and fungal (cryptococcal meningitis)
• Tuberculous meningitis occurs in children and adults through haematogenous spread of infection from tuberculosis
• Cryptococcal meningitis develops particularly in debilitated or immunocompromised persons, usually as a result of haematogenous dissemination from a pulmonary lesion
CLINICAL FEATURES AND DIAGNOSIS OF MENINGITIS
• Tuberculous meningitis manifests clinically as headache, confusion, malaise and vomiting
- Lumbar Puncture: A sample of cerebrospinal fluid (CSF) is taken from the lower back to check for signs of infection.
- Blood Tests: To identify the presence of bacteria or viruses in the bloodstream.
- Imaging: CT scans or MRIs may be used to detect any abnormalities in the brain or the meninges.
Treatment:
- Antibiotics: For bacterial meningitis, immediate antibiotic treatment is essential.
- Antiviral Medications: In the case of viral meningitis.
- Supportive Care: To manage symptoms, such as pain relief and hydration.
- Hospitalization: Severe cases often require hospitalization and close monitoring.
Prevention:
- Vaccination: Vaccines are available for some of the most common bacterial causes of meningitis, including Haemophilus influenzae type b, Neisseria meningitidis, and Streptococcus pneumoniae.
- Good Hygiene: Practicing proper hygiene, especially handwashing, can help prevent the spread of infections.
- Avoid Close Contact: During meningitis outbreaks, avoiding close contact with infected individuals is crucial.
Summary
• Meningitis is inflammatory involvement of the meninges
• Acute pyogenic or acute purulent meningitis is acute infection of the pia-arachnoid and of the CSF enclosed in the subarachnoid space
• Acute lymphocytic meningitis is a viral or aseptic meningitis, especially common in children and young adults.
• There are two principal types of chronic meningitis—bacterial (tuberculous meningitis) and fungal (cryptococcal meningitis)
Meningitis B Pharma 2nd Semester Pathophysiology notes pdf
Meningitis FAQ:
Q1: What is meningitis? Meningitis is an inflammation of the meninges, the protective membranes that cover the brain and spinal cord. It can be caused by infections, most commonly viruses and bacteria.
Q2: What are the common symptoms of meningitis? Common symptoms include high fever, severe headache, stiff neck, sensitivity to light (photophobia), nausea, vomiting, confusion, and in severe cases, seizures and a characteristic rash.
Q3: What are the main types of meningitis? There are three main types: viral, bacterial, and fungal meningitis. Bacterial meningitis is the most severe and life-threatening.
Q4: How is meningitis transmitted? Meningitis can be transmitted through respiratory droplets (coughing or sneezing) or direct contact with an infected person’s respiratory secretions or saliva.
Q5: Who is at risk for meningitis? Individuals at higher risk include those with weakened immune systems, close contacts of someone with bacterial meningitis, and individuals living in crowded or communal settings, such as college dormitories.
Q6: How is meningitis diagnosed? Diagnosis often involves a lumbar puncture (spinal tap) to collect cerebrospinal fluid for analysis, blood tests, and imaging (CT or MRI scans) to check for signs of infection.
Q7: Is meningitis contagious? Meningitis can be contagious, especially when it’s caused by infectious agents like viruses or certain bacteria. Close contact with an infected person can lead to transmission.
Q8: Can meningitis be prevented through vaccination? Yes, vaccines are available for some of the most common bacterial causes of meningitis, including Haemophilus influenzae type b, Neisseria meningitidis, and Streptococcus pneumoniae. These vaccines are vital for prevention.
Q9: What is the treatment for meningitis? The treatment depends on the type of meningitis. Bacterial meningitis requires immediate antibiotic therapy, while viral meningitis may be managed with supportive care. Hospitalization is often necessary for severe cases.
Q10: Are there long-term complications associated with meningitis? Meningitis can lead to long-term complications, such as hearing loss, neurological problems, and cognitive deficits, especially in severe cases.
Q11: Is there a vaccine for viral meningitis? There isn’t a specific vaccine for viral meningitis because it can be caused by a variety of viruses. However, some viral infections, like mumps and varicella-zoster, have vaccines to prevent the underlying diseases that could lead to viral meningitis.
Q12: Can you get meningitis more than once? It’s possible to get meningitis more than once, depending on the cause. For instance, recurrent viral meningitis can occur with different viral infections. Vaccination against bacterial causes can prevent recurrence of bacterial meningitis.
Q13: How can I reduce the risk of meningitis? Practicing good hygiene, getting vaccinated, and avoiding close contact with infected individuals can help reduce the risk of contracting meningitis.
Q14: Is there a specific age group most affected by meningitis? Meningitis can affect individuals of all ages. However, certain types, like meningococcal meningitis, are more common in adolescents and young adults
Also, Visit: B. Pharmacy Notes | B. Pharma Notes | Study material Bachelor of Pharmacy