Leprosy

• Caused by bacteria Mycobacterium leprae
• It causes damage to the skin and the peripheral nervous system.
• Disease develops slowly (from six months to 40 years)
• Results in skin lesions and deformities, most often affecting the cooler places on the body
• Skin, mouth, respiratory tract, eyes, peripheral nerves, superficial lymphnodes and testis
Signs of leprosy
• Pale or slightly reddish patch
• Definite loss of sensation in the patch
• Signs of damage to nerves
– Definite loss of sensation in cooler areas of body hands/feet
– Weakness of muscles of hands/feet/face
– Visible deformity of hands/feet/face
Symptoms of Leprosy
• Symptoms are similar to those that may occur with syphilis, tetanus
• Numbness and loss of temperature sensation (cannot sense very hot or cold temperatures)
• As the disease progresses, the sensations of touch, then pain, and eventually deep pressure are decreased or lost
Mode of transmission of Leprosy
• Slow communicable disease
• Incubation period between first exposure and appearance of signs of disease varies from 2- 20 years
• Direct contact with untreated leprosy patient – shed numerous bacilli from damaged skin, nasal secretions, mucus membrane of mouth and hair follicles
• Materno – foetal transmission across plancenta
• From milk of leprosy patient to infant
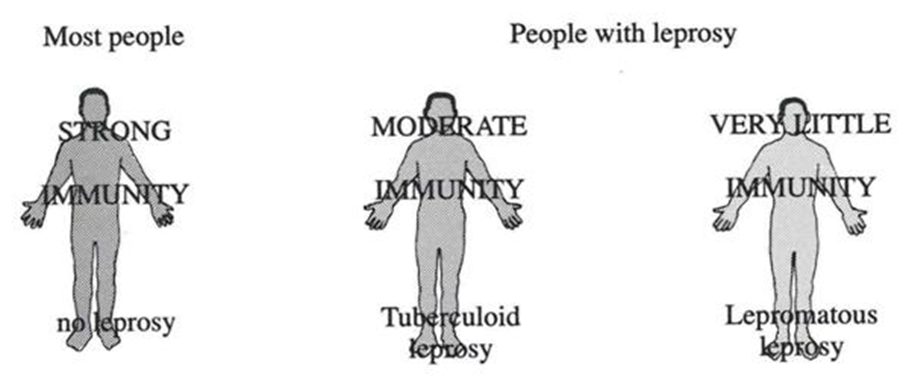
Types of leprosy
• Lepromatous leprosy
• Skin lesions are symmetrical, hypopigmented, erythomateous macules, nodules or diffuse infiltrates
• Lesions are anaesthetic, sensory disturbance not distinct as TT
• Tuberculoid leprosy
• Lesions are either single or as a symmetrical hypopigmented, erythematous macule
• Distinct sensory impairment
Pathophysiology of Leprosy
• Sebaceous glands and hair follicles
• Onset, small cutaneous nerve fibers are involved
• With bacillary multiplication, contiguous skin areas, including autonomic nerve fibers, dermal appendages, and blood vessels, are invaded
• As infection spreads along sensory nerves, motor fibers within parent nerve trunks are damaged
• Leprosy bacilli are unable to penetrate nervous system proximal to the dorsal root ganglions
• Central nervous system infection does not occur
• Little systemic reaction, and tissue destruction occurs mainly in cool, superficial locations: the skin (except in folds)
• Peripheral nerves in subcutaneous loci, oral and nasopharyngeal mucous membranes (not enteric or vaginal); the testes (not the ovaries); anterior third of the eye
Diagnosis of Leprosy
Clinical Examination: The first step in diagnosing leprosy involves a thorough clinical examination by a trained healthcare provider. They look for characteristic skin lesions, loss of sensation, and nerve involvement.
Skin Smear Test: A skin smear test involves taking a small sample from skin lesions to examine under a microscope. It helps identify the presence of acid-fast bacilli, indicating leprosy infection.
Biopsy: A skin biopsy may be performed to confirm the diagnosis and determine the specific type of leprosy.
Nerve Biopsy: Nerve involvement is common in leprosy. A nerve biopsy helps in assessing nerve damage and guiding treatment.
Treatment Options for Leprosy:
Multidrug Therapy (MDT): MDT is the primary and most effective treatment for leprosy. It involves combining three antimicrobial drugs: dapsone, rifampicin, and clofazimine. The duration of treatment varies based on the type and severity of leprosy.
Single Drug Therapy (SDT): For milder cases of leprosy, single drug therapy with rifampicin is sometimes used.
Steroids: In certain cases, corticosteroids may be prescribed to manage inflammatory reactions known as leprosy reactions.
Supportive Care: Patients may receive supportive care to manage any complications arising from leprosy, such as wound care for skin ulcers or physical therapy for nerve damage.
Summary
• Leprosy is a disease caused by the bacteria mycobacterium leprae and the disease develops slowly and results in skin lesions and deformities, most often affecting the cooler places
• Classified in to five types indeterminate leprosy, tuberculoid leprosy, borderline tuberculoid leprosy, lepromatous leprosy, mid borderline leprosy
• Leprosy have clinically detectable lesion all over the body with inolvement of sensory at first and motor fibres at the later stages with significant bactermia affecting every organ
Also, Visit: Health and Wellness