Respiratory system

Objectives
At the end of this lecture, student will be able to
• Enumerate structural classification
• Illustrate functional portions of respiratory system
• Describe the anatomy of the nose, pharynx.
• Describe the anatomy of the larynx, trachea
• Describe the structure involved in sound production
• Explain the process of breathing
• Discuss the structure of alveoli
• Outline lung volumes and capacities
• Describe the exchange of oxygen and carbon dioxide in
internal and external respiration
• Describe how the blood transports oxygen and carbon
dioxide
• Explain how the nervous system controls breathing
• Discuss different disorders of respiratory tract
Organization and Functions of the Respiratory System
Structural classifications:
– Upper respiratory tract
– Lower respiratory tract.
• Functional classifications:
– Conducting portion: transports air.
• Nose
• Nasal cavity
• Pharynx
• Larynx
• Trachea
• Progressively smaller airways, from the primary bronchi to the bronchioles
– Respiratory portion: carries out gas exchange.
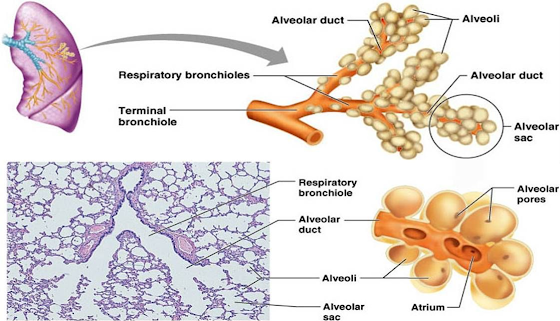
• Respiratory bronchioles
• Alveolar ducts
• Air sacs called alveoli
• Upper respiratory tract is all conducting
• Lower respiratory tract has both conducting and respiratory portions
Respiratory System Functions
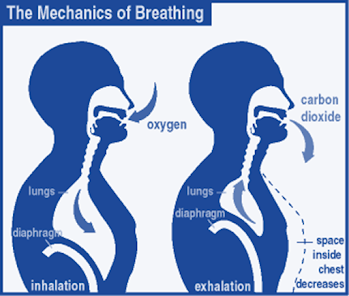
• Breathing (pulmonary ventilation):
– consists of two cyclic phases:
• Inhalation, also called inspiration
• Exhalation, also called expiration
– Inhalation draws gases into the lungs.
– Exhalation forces gases out of the lungs.
• Gas exchange: O2 and CO2
– External respiration
• External environment and blood
– Internal respiration
• Blood and cells
• Gas conditioning:
– Warmed
– Humidified
– Cleaned off particulates
• Sound production:
– Movement of air over true vocal cords
– Also involves nose, paranasal sinuses, teeth, lips and tongue
• Olfaction:
– Olfactory epithelium over superior nasal conchae
• Defense:
– Course hairs, mucus, and lymphoid tissue
Upper Respiratory Tract
• Composed of
– The nose
– The nasal cavity
– The paranasal sinuses
– The pharynx (throat)
– And associated structures.
• All part of the conducting portion of the respiratory system.
Paranasal Sinuses
• Paranasal sinuses:
– In four skull bones
– paired air spaces
– decrease skull bone weight
• Named for the bones in which they are housed.
– Frontal
– ethmoidal
– sphenoidal
– Maxillary
• Communicate with the nasal cavity by ducts.
• Covered with the same pseudostratified ciliated columnar epithelium as the nasal cavity.
Pharynx
• Common to both the respiratory and digestive systems.
• Commonly called the throat.
• Funnel-shaped – Slightly wider superiorly and narrower inferiorly.
• Originates posterior to the nasal and oral cavities
• Extends inferiorly near the level of the bifurcation of the larynx and esophagus.
• Common pathway for both air and food.
• Walls:
– lined by a mucosa
– contain skeletal muscles primarily used for swallowing.
• Flexible lateral walls
– Distensible
– To force swallowed food into the esophagus.
• Partitioned into three adjoining regions:
– Nasopharynx
– Oropharynx
– Laryngopharynx
Nasopharynx
• Superiormost region of the pharynx.
• Location:
– Posterior to the nasal cavity
– Superior to the soft palate
• separates it from the posterior part of the oral cavity.
• Normally, only air passes through.
• Soft palate
– Blocks material from the oral cavity and oropharynx
– elevates when we swallow.
• Auditory tubes
– paired
– In the lateral walls of the nasopharynx
– connect the nasopharynx to the middle ear.
• Pharyngeal tonsil
– Posterior nasopharynx wall
– Single
– Commonly called the adenoids.
Oropharynx
• The middle pharyngeal region.
• Location:
– Immediately posterior to the oral cavity.
– Bounded by the soft palate superiorly,
– The hyoid bone inferiorly.
• Common respiratory and digestive pathway
– Both air and swallowed food and drink pass through.
• 2 pairs of muscular arches
– Anterior palatoglossal arches
– Posterior palatopharyngeal arches
– Form the entrance from the oral cavity.
• Lymphatic organs
– provide the first line of defense against ingested or inhaled foreign materials.
• Palatine tonsils – On the lateral wall between the arches
• Lingual tonsils – At the base of the tongue.
Laryngopharynx
• Inferior, narrowed region of the pharynx.
• Location:
– Extends inferiorly from the hyoid bone
– is continuous with the larynx and esophagus.
– Terminates at the superior border of the esophagus
• is equivalent to the inferior border of the cricoid cartilage in the larynx.
• The larynx (voice box) forms the anterior wall
• Lined with a nonkeratinized stratified squamous epithelium (mucus membrane)
• Permits passage of both food and air.
Lower Respiratory Tract
• Conducting portion
– Larynx
– Trachea
– Bronchi
– Bronchioles and their associated structures
• Respiratory portion of the respiratory system
– Respiratory bronchioles
– Alveolar ducts
– Alveoli
Larynx
• Short, somewhat cylindrical airway
• Location:
– Bounded posteriorly by the laryngopharynx,
– Inferiorly by the trachea.
• Prevents swallowed materials from entering respiratory tract.
• Conducts air into the lower respiratory tract.
• Produces sounds.
• Nine pieces of cartilage
– Three individual pieces
• Thyroid cartilage
• Cricoid cartilage
• Epiglottis
– Three cartilage pairs
• Arytenoids: on cricoid
• Corniculates: attach to arytenoids
• Cuniforms: in aryepiglottic fold
– held in place by ligaments and muscles.
• Intrinsic muscles: regulate tension on true vocal cords
• Extrinsic muscles: stabilize the larynx
Sound Production
• Two pairs of ligaments
• Inferior ligaments, called vocal ligaments
– covered by a mucous membrane
– Vocal folds: ligament and mucosa.
– are true vocal cords
• They produce sound when air passes between them
• Superior ligaments, called vestibular ligaments
– Covered by mucosa
– Vestibular folds: ligament and mucosa
– Are false vocal cords
• No function in sound production
• protect the vocal folds.
– The vestibular folds attach to the corniculate cartilages.
• The tension, length, and position of the vocal folds determine the quality of the sound.
– Longer vocal folds produce lower sounds
– More taunt, higher pitch
– Loudness based on force of air
• Rima glottidis: opening between the vocal folds
• Glottis: rima glottidis and the vocal folds
Trachea
• A flexible, slightly rigid tubular organ
– Often referred to as the windpipe.
• Extends through the mediastinum
– Immediately anterior to the esophagus
– Inferior to the larynx
– Superior to the primary bronchi of the lungs.
• Anterior and lateral walls of the trachea are supported by 15 to 20 C-shaped tracheal cartilages.
– Cartilage rings reinforce and provide some rigidity to the tracheal wall to ensure that the trachea remains open (patent) at all times
– Cartilage rings are connected by elastic sheets called anular ligaments.
• At the level of the sternal angle, the trachea bifurcates into two smaller tubes, called the right and left primary bronchi.
• Each primary bronchus projects laterally toward each lung.
• The most inferior tracheal cartilage separates the primary bronchi at their origin and forms an internal ridge called the carina.
Bronchial Tree
• A highly branched system
– Air-conducting passages
– originate from the left and right primary bronchi.
• Progressively branch into narrower tubes as they diverge throughout the lungs before terminating in terminal bronchioles.
• Primary bronchi
– Incomplete rings of hyaline cartilage ensure that they remain open.
– Right primary bronchus
• Shorter, wider, and more vertically oriented than the left primary bronchus.
– Foreign particles are more likely to lodge in the right primary bronchus.
– enter the hilum of each lung
– Also entering hilum:
• Pulmonary vessels
• Lymphatic vessels
• Nerves.
• Secondary bronchi (or lobar bronchi)
– Branch of primary bronchus
– Left lung:
• Two lobes
• Two secondary bronchi
– Right lung
• Three lobes
• Three secondary bronchi.
• Tertiary bronchi (or segmental bronchi)
– Branch of secondary bronchi
– Left lung is supplied by 8 to 10 tertiary bronchi.
– Right lung is supplied by 10 tertiary bronchi
– Supply a part of the lung called a bronchopulmonary segment.
Respiratory Bronchioles, Alveolar Ducts, and Alveoli
• Contain small saccular outpocketings called alveoli.
• An alveolus is about 0.25 to 0.5 millimeter in diameter.
• Its thin wall is specialized to promote diffusion of gases between the alveolus and the blood in the pulmonary capillaries.
• Gas exchange can take place in the respiratory bronchioles and alveolar ducts as well as in the lungs, which contain approximately 300–400 million alveoli.
• The spongy nature of the lung is due to the packing of millions of alveoli together.
Gross Anatomy of the Lungs
• Each lung has a conical shape.
• Its wide, concave base rests upon the muscular diaphragm.
• Its relatively blunt superior region, called the apex or (cupola), projects superiorly to a slightly superior point and posterior to the clavicle.
• Both lungs are bordered by the thoracic wall anteriorly, laterally, and posteriorly, and supported by the rib cage.
• Toward the midline, the lungs are separated from each other by the mediastinum.
• The relatively broad, rounded surface in contact with the thoracic wall is called the costal surface of the lung.
Pleura and Pleural Cavities
• The outer surface of each lung and the adjacent internal thoracic wall are lined by a serous membrane called pleura, which is formed from simple squamous epithelium.
• The outer surface of each lung is tightly covered by the visceral pleura, while the internal thoracic walls, the lateral surfaces of the mediastinum, and the superior surface of the diaphragm are lined by the parietal pleura.
• The parietal and visceral pleural layers are continuous at the hilum of each lung.
• The outer surface of each lung is tightly covered by the visceral pleura, while the internal thoracic walls, the lateral surfaces of the mediastinum, and the superior surface of the diaphragm are lined by the parietal pleura.
• The potential space between these serous membrane layers is a pleural cavity.
• The pleural membranes produce a thin, serous fluid that circulates in the pleural cavity and acts as a lubricant, ensuring minimal friction during breathing.
Lymphatic Drainage
• Lymph nodes and vessels are located within the connective tissue of the lung as well as around the bronchi and pleura.
• The lymph nodes collect carbon, dust particles, and pollutants that were not filtered out by the pseudostratified ciliated columnar epithelium.
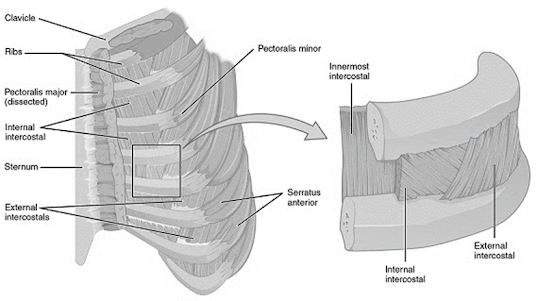
Thoracic Wall Dimensional Changes during Respiration
• Lateral dimensional changes occur with rib movements.
• Elevation of the ribs increases the lateral dimensions of the thoracic cavity, while depression of the ribs decreases the lateral dimensions of the thoracic cavity.
Mechanism of Respiration
Muscles that Move the Ribs
• The scalenes help increase thoracic cavity dimensions by elevating the first and second ribs during forced inhalation.
• The ribs elevate upon contraction of the external intercostals, thereby increasing the transverse dimensions of the thoracic cavity during inhalation.
• Contraction of the internal intercostals depresses the ribs, but this only occurs during forced exhalation.
• Normal exhalation requires no active muscular effort.
• A small transversus thoracis extends across the inner surface of the thoracic cage and attaches to ribs 2–6. It helps depress the 23 ribs.
• Two posterior thorax muscles also assist with respiration. These muscles are located deep to the trapezius and latissimus dorsi, but superficial to the erector spinae muscles.
• The serratus posterior superior elevates ribs 2–5 during inhalation, and the serratus posterior inferior depresses ribs 8–12 during exhalation.
• In addition, some accessory muscles assist with respiratory activities.
• The pectoralis minor, serratus anterior, and sternocleidomastoid help with forced inhalation, while the abdominal muscles (external and internal obliques, transversus abdominis, and rectus abdominis) assist in active exhalation.
Boyle’s Law
• The pressure of a gas decreases if the volume of the container increases, and vice versa.
• When the volume of the thoracic cavity increases even slightly during inhalation, the intrapulmonary pressure decreases slightly, and air flows into the lungs through the conducting airways.
• Air flows into the lungs from a region of higher pressure (the atmosphere) into a region of lower pressure (the intrapulmonary region).
• When the volume of the thoracic cavity decreases during exhalation, the intrapulmonary pressure increases and forces air out of the lungs into the atmosphere.
Ventilation Control by Respiratory Centers of the Brain
• The trachea, bronchial tree, and lungs are innervated by the autonomic nervous system.
• The autonomic nerve fibers that innervate the heart also send branches to the respiratory structures.
• The involuntary, rhythmic activities that deliver and remove respiratory gases are regulated in the brainstem.
• Regulatory respiratory centers are located within the reticular formation through both the medulla oblongata and pons.
Aging and the Respiratory System
• Becomes less efficient with age due to several structural changes.
• Decrease in elastic connective tissue in the lungs and the thoracic cavity wall.
• Loss of elasticity reduces the amount of gas that can be exchanged with each breath and results in a decrease in the ventilation rate.
• Emphysema may cause a loss of alveoli or their functionality
• Reduced capacity for gas exchange can cause an older person to become short of breath upon exertion.
• Carbon, dust, and pollution material gradually accumulate in our lymph nodes and lungs.
Respiratory Regulation during Exercise
Pulmonary Ventilation
– Commonly referred to as breathing
– Process of moving air in and out of the lungs
– Nasal breathing: warms, humidifies, and filters the air we breathe
– Pleural sacs suspend the lungs from the thorax and contain fluid to prevent friction against the thoracic cage.
Bronchial tree
Intercostal muscles
The composition of inspired and expired air
| Inspired air % | Expired air % |
Oxygen | 21 | 16 |
Carbon dioxide | 0.04 | 4 |
Nitrogen and rare gases | 74 | 78 |
Water vapour | Variable | Saturated |
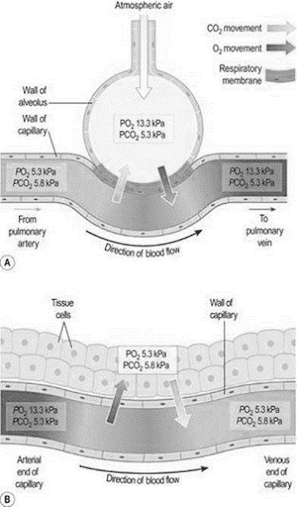
Partial pressures of gases
Gas | Alveolar | Deoxygenated | Oxygenated | |||
kPa | mmHg | kPa | mmHg | kPa | mmHg | |
Oxygen | 13.3 | 100 | 5.3 | 40 | 13.3 | 100 |
Carbon dioxide | 5.3 | 40 | 5.8 | 44 | 5.3 | 40 |
Nitrogen and other inert gases | 76.4 | 573 | 76.4 | 573 | 76.4 | 573 |
Water vapour | 6.3 | 47 | ||||
Total = | 101.3 | 760 | ||||
External and Internal Respiration-Mechanism
Pulmonary Ventilation
• Inspiration
– is an active process of the diaphragm and the external intercostal muscles.
– Air rushes in into the lungs to reduce a pressure difference.
– Forced inspiration is further assisted by the scalene, sternocleidomastoid, and pectoralis muscles.
• Expiration
– is a passive relaxation of the inspiratory muscles and the lung recoils.
– increased thoracic pressure forces air out of the lungs
– Forced expiration is an active process of the internal intercostal muscles (latissimus dorsi, quadratus lumborum & abdominals).
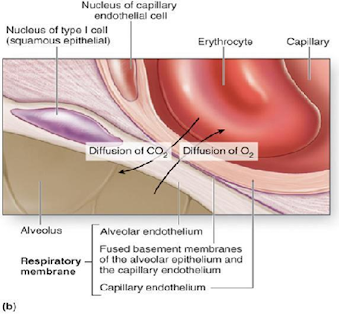
Pulmonary Diffusion
• Is the gas exchange in the lungs and serves two functions:
– It replenishes the blood’s oxygen supply in pulmonary capillaries
– It removes carbon dioxide from the pulmonary capillaries
• The respiratory membrane
– Gas exchange occurs between the air in the alveoli, through the respiratory membrane, to the red blood cells in the blood of the pulmonary capillaries.
• Partial Pressures of gasses
– The individual pressures from each gas in a mixture together create a total pressure.
– Air we breathe = 79% (N2), 21% (O2), and .03% (CO2) = 760mmHg
– Differences in the partial pressures of the gases in the alveoli and the gases in the blood create a pressure gradient.
• OdžLJgen’s rate at which it diffuses from the alveoli into the blood is referred to as the oxygen diffusion capacity.
• Untrained (45 ml/kg /min) vs trained (80 ml/kg /min) – Due to increased cardiac output, alveolar surface area, and reduced resistance to diffusion across the respiratory membranes.
• Large athletes (males) vs small athletes (females) – Due to increased lung capacity, increased alveolar surface area, and increased blood pressure from muscle pumping.
Carbon diodžide’s membrane solubility is 20 times greater than that of oxygen, so CO2 can diffuse across the respiratory membrane much more rapidly.
Transport of Oxygen by the Blood
• Dissolved in the blood plasma (2%)
• Dissolved with hemoglobin of red blood cells (98%)
– Complete hemoglobin saturation at sea level is 98%.
– Many factors influence hemoglobin saturation
• Po2 values
• Decline in pH level from increasing lactate levels allows more oxygen to be unloaded and higher Po2 is needed to saturate the hemoglobin.
• Increased blood temperature allows oxygen to unload more efficiently and higher Po2 is needed to saturate the hemoglobin.
• Anemia reduces the blood’s oxygen-carrying capacity.
Transport of Carbon Dioxide in the Blood
• CO2 released from the tissues is rarely (7%) dissolved in plasma.
• CO2 combines with H2O, then loses a H+ ion to form a bicarbonate ion (HCO3) and transports 70% of carbon dioxide back to the lungs.
– The lost H+ binds to hemoglobin which enhances oxygen unloading
– Sodium bicarbonate as an ergogenic aid serves the same purpose as a buffer and neutralizer of H+ preventing blood acidification.
• CO2 can also bind with the amino acids of the hemoglobin to 10
Regulation of Pulmonary Ventilation
• Mechanisms of pulmonary ventilation
– controlled by respiratory centers of the brainstem by sending out periodic impulses to the respiratory muscles.
– Chemoreceptors also stimulate the brain to stimulate the respiratory centers to increase respiration to rid the body of carbon dioxide.
– Stretch receptors of the pleurae, bronchioles and alveoli send impulses to the expiratory center to shorten inspiration.
– The motor cortex of the voluntary nervous system can control ventilation but can also be overriden by the involuntary system.
Regulatory centres of Respiration
Respiratory Limitations to Performance
• Energy produced by oxidation and used by the respiratory muscles increases from 2% to 15% during heavy exercise.
• Pulmonary Ventilation might be a limiting factor in highly trained subjects during maximal exhaustive exercise due to a high Vo2 max.
• Airway Resistance and Gas Diffusion in the lungs do not limit exercise in a normal healthy individual.
• Restrictive or Obstructive Air Ways can limit athletic performance by decreasing the Po2 or increasing the Pco2.
– Asthma
– Bronchitis
– Emphysema
Respiratory Regulation of Acid-Base Balance
• Chemical Buffers
– Bicarbonate, phosphates, and proteins
– Increased ventilation to decrease H+
– Accumulated H+ is removed by the kidneys and urinary system
– H+ is difused throughout the body fluids and reach equilibrium after only 5 to 10 minutes of recovery
• This is facilitated by active recovery.
Static Lung Volumes
• Total Lung Capacity
• Tidal Volume
• Inspiratory Reserve Volume
• Expiratory Reserve Volume
• Residual Lung Volume
• Forced Vital Capacity
• Inspiratory Capacity
• Functional Residual Volume
Lung volumes and capacities
• Anatomical dead space- As the exchange of gases takes place only across the walls of the alveolar ducts and alveoli, the remaining capacity of the respiratory passage is Anatomical dead space (150ml)
• Tidal Volume- Amount of air passing into and out of lungs during each breath (500ml at rest)
• Inspiratory Reserve Volume- Extra volume of air that can be inhaled into the lungs during maximal inspiration
• Expiratory Reserve Volume – Largest volume of air which can be expelled from the lungs during maximal respiration
• Residual Lung Volume – volume of air remaining in the lungs after forced expiration
• Vital Capacity =TV+IRV+ERV
• Inspiratory Capacity – Amount of air that can be inspired with maximum effort (TV+IRV=500ml)
• Functional Residual Volume- Amount of air remaining in the air passages and alveoli at the end of the respiration.
• Alveolar Ventilation- Volume of air that moves into and out of the alveoli per minute (TV – ADS X Respiratory rate) (500-150 X 15=5.25litres/min
Common Disorders of Respiratory System
• URI – Upper Respiratory Infection – infection of nose, throat, larynx, trachea
• Pneumonia – inflammation or infection of the lungs
• Emphysema (Chronic Obstructive Pulmonary Disease – COPD) – alveoli become stretched and stiff preventing adequate exchange of oxygen and carbon dioxide
• Asthma – spasms of bronchial tube walls causing narrowing of air passages usually due to allergies
• Allergy – reaction to substances that leads to slight or severe response by body.
• Influenza – highly contagious URI
• Pleurisy – inflammation of the pleura surrounding the l
• Bronchitis – inflammation of the bronchi
• Lung cancer – malignant tumors in the lungs that destroy tissue
Changes in Respiratory System – Due To Aging
• Lung tissue becomes less elastic
• Respiratory muscles weaken
• Number of alveoli decrease
• Respirations increase
• Voice pitched higher and weaker due to changes in larynx
• Chest wall and structures become more rigid
Observations of Respiratory System
• Rate and rhythm of respirations
• Respiratory secretions – character
• Character of cough
• Changes in skin color – pale or bluish gray
• Temperature changes
• Difficulty breathing
• Color of sputum
• Complaint of pain in chest, back, sides
• Shortness of breath
• Noisy respirations
• Sneezing
• Gasping for breath
• Anxiety
Summary
• Respiratory System structurally divided into Upper and lower respiratory tract
• Respiratory System functionally divided into Conducting and respiratory portion
• The human respiratory system is a series of organs responsible for taking in oxygen and expelling carbon dioxide. The primary organs of the respiratory system are lungs, which carry out this exchange of gases
• Breathing – Two cyclic phases – Inhalation and exhalation
• Gas exchange takes – External and Internal respiratory mechanisms
• Main functions of respiratory system – Gas conditioning, Sound production, Olfaction and Defense
• Gas exchange – It takes place in the respiratory bronchioles, alveolar ducts and in the lungs
• Inhalation – External intercostal muscle contract and elevate the ribs.
• As the diaphragm contracts, the rib cage is simultaneously enlarged by the ribs being pulled upwards by the intercostal muscles
• Normal exhalation requires no active muscular effort
• The trachea, bronchial tree, and lungs are innervated by the autonomic nervous system
• Regulatory respiratory centers are located within the reticular formation through both the medulla oblongata and pons
• Regulatory respiratory centers are located within the reticular formation through both the medulla oblongata and pons.
• COPD, Asthma, Bronchitis are common disorders of respiratory tract.
• Tidal volume, vital capacity all are important for measurement of total lung capacity
Also, Visit:
B. Pharma Notes | B. Pharma Notes | Study material Bachelor of Pharmacy pdf