Alzheimer’s disease
Objectives
By the end of this session, students will be able to:
a) Explain the pathophysiology of Alzheimer’s Disease
b) Explain the pharmacology of drugs used in Alzheimer’s Disease
c) Discuss the treatment of Alzheimer’s Disease
d) Enumerate the adverse effects of drugs used in the treatment of Alzheimer’s Disease
Alzheimer’s disease
· Alzheimer’s disease (AD), first characterized by Alois Alzheimera, a German psychiatrist and neuropathologist in 1907 and is a gradually progressive dementia affecting both cognition and behavior
· ‘Also known as Senile Dementia of the Alzheimer Type (SDAT)
· A slowly progressive disease of the brain that is characterized by impairment of memory and eventually by disturbances in reasoning, planning, language, and perception
· Many scientists believe AD results from an increase in the production or accumulation of a specific protein (beta-amyloid protein) in the brain leading to nerve cell death
Epidemiology of Alzheimer’s disease
· Disease responsible for 55% of the total causes of dementia
· Survival following AD onset estimated to be 3 to 20 years, with an average of 8 years
· Known to have affected 35.8 million people in the world and this number is expected to increase by 1/4th by 2050
· The most prevalent cause of deaths in adults after heart disease, cancer and stroke
Etiology of Alzheimer’s disease
· Although dementia syndrome may be caused by 60 other disorders, most cases are due to Alzheimer’s followed by multi infarct dementia or combination of both
· The putative risk factors for the Alzheimer’s dementia include advancing age, a history of serious head trauma, hypothyroidism, dementia in a first circle relative and down’s syndrome in a first circle relative
· Alzheimer’s disease is correlated with diminished neuron function and decreased neurotransmitters
· The major abnormality observed in the Alzheimer’s is a 40-90% decrease in the enzyme choline acetyl esterase in the cerebral cortex and the hippocampus
· Although acetylcholine is the major neurotransmitter deficit associated, other neurotransmitters like somatostatin and corticotrophin-releasing factors are also found to be decreased
Pathogenesis of Alzheimer’s disease
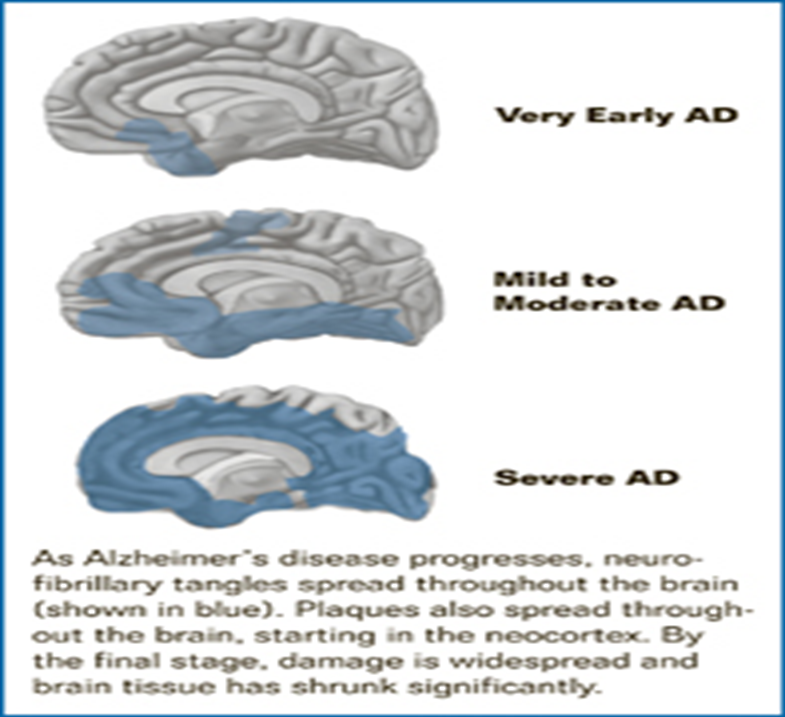
Ø Brain autopsy studies revealed that Alzheimer’s patients have cortical atrophy, a significant loss of neurons, an increase in the neuritic plaques and a high density of neurofibrillary tangles.
Neuropathologically AD destroys neurons in the cortex and limbic areas of the brain such as:
• The basal forebrain, amygdala, hippocampus, and cerebral cortex
• These areas are responsible for higher learning, memory, reasoning, behaviour, and emotional control
Anatomically, four major alterations in brain structure are seen:
• Cortical atrophy, degeneration of cholinergic and other neurons, presence of neurofibrillary tangles (NFTs), and the accumulation of neuritic plaques
• The signature lesions of AD are NFTs and neuritic plaques
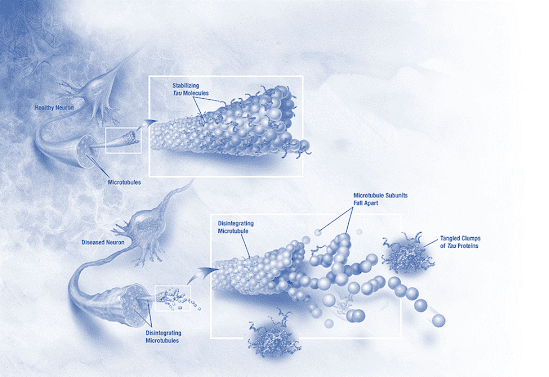
Neuro fibrillary Tangles
• Aggregates of hyper phosphorylated tau protein
• Tau protein provides structural support to microtubules
• Aggregations of hyper phosphorylated tau protein are also referred to as PHF, or “paired helical filaments
• When tau filaments undergo abnormal phosphorylation at a specific site, they cannot bind effectively to microtubules, and the microtubules collapse
• Without an intact system of microtubules, the cell cannot function properly and eventually dies
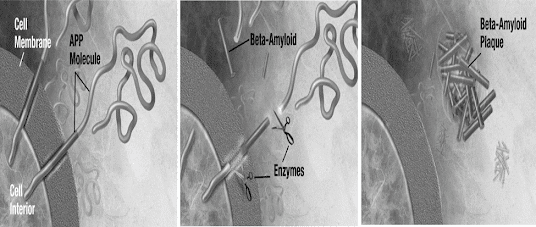
Neuritic plaques
• Extracellular deposits of beta amyloid (a 39- to 43-amino acid protein segment) in the gray matter of the brain
• Primarily composed of beta amyloid peptides and an entwined mass of broken neurites (axon and dendrite projections of neurons)
• These polypeptides tend to aggregate and are neurotoxic
• Plaques are variable in shape and size, but are on average 50 µm in size
• Accumulation of aggregated amyloid fibrils disrupts the cell’s calcium ion homeostasis and utilization of glucose by neurons inducing apoptosis
• The βAP also accumulate in the brain and cerebral blood vessels
• Two types of glial cells, astrocytes and microglia, also found in plaques
• Glial cells also secrete inflammatory mediators and serve as scavenger cells, which may be important in causing the inflammatory processes that occur in the development of AD
• Enzymes act on the APP (amyloid precursor protein) and cut it into fragments
• The beta-amyloid fragment is crucial in the formation of senile plaques in AD
• Inflammatory Mediators- increased presence of APP (Amyloid Precursor Protein), α1-antichromotrypsin and α2-macroglobulin, in the serum and within amyloid plaques of patients with AD has been proved
• α1-antichromotrypsin and α2-macroglobulin act as protease inhibitors affecting proteolytic breakdown of βAP
• Inflammatory mediators increase βAP toxicity and aggregation
• The complement-derived Membrane Attack Complex, is found associated with broken neurites and areas containing NFTs
The cholinergic system-
• Damage occurs in any nerve cell population located in or traveling through plaque laden areas
• Cholinergic neurons located at the base of the forebrain in the nucleus basalis of Meynert, a brain area involved in thought integration is profoundly damaged
• Axons of these cholinergic neurons project to the frontal cortex and hippocampus, areas strongly associated with memory and cognition
Other neurotransmitter abnormalities-
• Serotonergic neurons of the raphe nuclei and noradrenergic cells of the locus ceruleus are lost
• Mao B activity is increased
• Abnormalities appear in glutamate pathways of the cortex and limbic structures (If glutamate is allowed to remain in the synapse for extended periods of time, it can destroy nerve cells)
Estrogen-
· Promotes neuronal growth, prevents oxidative damage, benefiting cells exposed to βAP
· Important in maintaining normal cholinergic neurotransmission
· Estrogen receptors are present in the hippocampus, cerebral cortex, and basal forebrain
· Estrogen receptors colocalize with receptors for nerve growth factor on cholinergic nerve terminals
· Estrogen supplementation also prevents decrements in choline uptake and choline acetyltransferase concentrations
· Thus estrogen is important in maintaining normal cholinergic neurotransmission
· May also increase NMDA receptor numbers in brain areas involved in recording new memories
· Prevents cell damage by acting as an antioxidant
Role of Apo lipo protein E and cholesterol
· Current research reveals the role for Apo lipo protein E(Apo E) in the pathogenesis of Alzheimer’s disease
· Apo E binds to the β-amyloid in the neurotic plaques and tangles
·
Identification
of this ApoE4 allele may eventually be used as a diagnostic aid or may be used
for pre-symptomatic testing for the Alzheimer’s disease
· Cholesterol depletion can inhibit the amyloidogenic pathway and prevent or slow down the plaque formation process
Stages of Alzheimer’s disease:
Symptoms of developing Alzheimer’s disease:
Early stage:
· A mild/early stage with duration period 2-4 years
· Frequent recent memory loss, particularly of recent conversations and events
· Repeated questions, some problems expressing and understanding language
· Writing and using objects become difficult and depression and apathy occur
· Drastic personality changes may accompany functional decline
· Need reminders for daily activities and difficulties with sequencing impact driving early in this stage
Second stage:
· Memory impairment progresses and early deficits of the early stage becomes more pronounced
· Decreased performance in the demanding employment or social situations
· Blunting of emotions and apathy common
· Judgement, the capacity for abstract thinking and calculations begin to wane or are lost
· Patients have difficulty in finding words and names
· Prevalence of agitation which can be aggressive/non-aggressive, physical or verbal, can increase with disease progression
· Psychotic symptoms like hallucinations, delusions and paranoia more become more prevalent towards the end of this stage
· Patients often become disoriented, lost, or wander and independent living becomes hazardous
Final stage:
· There is disturbance of practically all intellectual functions
· Patients are disoriented and incapacitated
· Activities of daily living is so impaired that independent living becomes hazardous
· Marked neurologic deficits and often increased muscle tone, akinesia, resulting in a slow and unsteady gait
· Loss of former personality traits
· Patients often fail to recognize relatives or even forget their own names
· Eventually become bedfast, become incontinent of the bowel and bladder
· Death is usually the result of pneumonia or other infections
Diagnosis of Alzheimer’s disease:
· Usually diagnosed clinically from the patient history, collateral history from relatives, and clinical observations, based on the presence of characteristic neurological and neuropsychological features and the absence of alternative conditions
· CT or MRI
· Positron Emission Tomography (PET)
· Neuropsychological tests such as the mini-mental state examination (MMSE) are widely used to evaluate the cognitive impairments needed for diagnosis.
· Psychological tests for depression are employed, since depression can either be concurrent with AD, an early sign of cognitive impairment, or even the cause
Treatment of Alzheimer’s disease:
Ø Two basic divisions of Alzheimer’s drug treatment
- First division and most often used is symptomatic drugs that are palliative and help to control unwanted behaviours and maintain patient’s normal functioning. These drugs primarily consist of psychotropic agents.
- The other division is therapeutic drugs. These agents are used to stop or reverse the disease process
and are largely experimental.
Primary goal
• To symptomatically treat cognitive difficulties and preserve patient function as long as possible
Secondary goal
• Treating the psychiatric and behavioral sequelae that occur as a result of the disease
Nonpharmacologic Therapy/ Basic Principles of Care for the Alzheimer’s Patient
Symptomatic Treatment of Alzheimer’s disease
1. Antidepressants:
· Early stages of Alzheimer’s often accompanied by depressive symptoms which may respond to drug therapy
· Resolution of the depression results in improvement of mood, functional abilities, and possibly cognitive functions
· All patients with dementia should be carefully evaluated for depression
· Depressive symptoms such as agitation, memory loss and insomnia can be easily confused with dementia
· Tricyclic antidepressants
· Newer Serotonin Specific Reuptake Inhibitors
· Atypical antidepressants
· For depressed Alzheimer’s patients who do not respond to tricyclics, SSRIs and other standard antidepressants or those who suffer from troublesome side effects the use of MAOIs should be considered
Classification of anti-depressants:
A) Monoamine oxidase inhibitors:
e.g. Hydrazines, Phenelzine, Clorgiline, selegiline, meclobemide
MOA:
· MAOI increase the concentration of NE, 5HT, DA within the normal synapse through inhibition of the MAO enzyme.
· Chronic therapy of MAOI causes changes in receptor sensitivity.
Drug interaction:
· Cheese
· Cold cough remedies
· Reserpine and levodopa.
These are metabolized in liver and excreted through urine.
Adverse effect:
· Fatigue
· Irritability
· tremor
· Insomnia
· Headache
· Dizziness
· Weight gain
· Blurred vision
· constipation
B) Tricyclic’s:
- Noradrenaline and serotonin reuptake inhibitors: these inhibit the re uptake of NA, and 5HT- e.g. Imipramine, Amitrptyline, Doxepine, clomipramine
- Noradrenaline re uptake inhibitor: Inhibits the reuptake of NA.
e.g. Nortyptyline, protryptiline, Amoxapine
- Selective serotonin re uptake inhibitors: Fluoxetine, paroxetine, Fluvoxamine
- Atypical anti-depressants: Trazadone, Bupropion, Mianserin, Nefazodone
Adverse effects
· Dry mouth
· Bad taste
· Constipation
· Epigastric distress
· Palpitation
· Blurred vision
· Sedation
· weakness
2. Hypnotics
· Insomnia is a common complaint among the elderly and it is even more prevalent in demented patients
· Sleep disturbances can be manifested by patients being awake at night, trying to go outside, or searching for lost items
· At such times hypnotics are given
· Sedating antidepressants trazadone 25 to 50mg at bedtime may be beneficial
· The short acting benzodiazepines triazolam, temazepam and zolpidem are often helpful
· Should be judiciously used because they can increase confusion and memory impairment, worsen depressive symptoms and aggrevate most other cognitive functions related to Alzheimer’s
· Chloral hydrate has been used in low doses
· Has many side effects too and more drug interactions than benzodiazepines, caution has to be taken because this drug can exacerbate symptoms of Alzheimer’s
· Diphenhydramine, used for its moderate sedating properties but has anticholinergic effects that may increase confusion and psychotic symptoms
· Alcohol intake has to be stopped or kept at very minimum level because of its effects on cognition, disruption of sleep pattern and other side effects
3. Anxiolytics
· Anxiety frequently affects patients with memory loss
· Judicious use of benzodiazeoines and buspirone in treating these symptoms has been successful
· Buspirone effective for the anxiety and mild agitation of the Alzheimer’s disease and has minimal side effects
4. Neuroleptics
· Indicated for specific psychotic symptoms such as auditory and visual hallucination, paranoia, and delusions with suspiciousness and severe agitation, which are stressful for the patients
· Do not affect higher cortical functions such as memory, judgement, and problem solving
· High potency anti-psychotics (haloperidol, fluphenazine) leave the patient prone to extrapyramidal side effects such as parkinsonism and tardive dyskinesia
· Low potency (chlorpromazine, thioridazine) are anti cholinergic and have cardiovascular side effects
· Low doses(haloperidol 0.5-1mg) given once or twice a day are usually sufficient
· The newer atypical antipsychotics(risperidone and clozaril) with effects on dopamine and serotonin have also been beneficial but may have extrapyramidal side effect profile
· A late afternoon or early evening dose may lessen the day time sedation and decrease “sundowning”
· The benefits of these psychotropic medications are variable and individualised effects are seen and also are limited by the side effects
· These drugs are useful and can improve behaviour functioning, easing the patient’s distress
· Antipsychotics have severe and permanent side effects and their use must be minimised. It is indicated only for those symptoms that are harmful and distressing to the patients that cannot be controlled through other means
· Because the disease is progressive, therapy should be evaluated at least every 6 months to ensure that the fewest drugs are being used in the lowest effective doses
Representative doses of psychotropic medications in Alzheimer’s disease:
Antidepressants:
| DRUG | DOSE |
| Fluoxetin | 10mg |
| Nortriptyline | 10mg |
| Paroxetin | 10mg |
| Phenelzine | 15mg |
| Sertaline | 25mg |
Anxiolytics:
| DRUG | DOSE |
| Alprazolam | 0.25mg |
| Buspirone | 5mg |
| Lorazepam | 0.5mg |
| Oxazepam | 10mg |
Antipsychotics:
| DRUG | DOSE |
| Clozapine | 25mg |
| Haloperidol | 0.5mg |
| Risperidone | 1mg |
| Thioridazine | 10mg |
| Thiothixene | 1mg |
Hypnotics:
| DRUG | DOSE |
| Chloral hydrate | 250-500mg |
| Temazepam | 7.5mg |
| Triazolam | 0.125mg |
| Zolpidem | 5mg |
Therapeutic treatment of Alzheimer’s disease
These drugs are being developed to slow progression of brain failure or reverse or alleviate disease symptoms in Alzheimer’s disease patients
1. Metabolic Enhancers
Ø Ergoloid mesylates FDA approved for use in the cognitive decline of the elderly
Ø A mixture of the methane sulfonate salts of three dihydrogenated ergot alkaloids (dihydroergocristine, dihydroergocornine, and alpha- and beta-dihydroergocryptine)
Ø Originally thought to act as a cerebral vasodilator, ergoloid mesylates are now classified as metabolic enhancers
Ø Modulate synaptic neurotransmission
Ø Alters glucose and oxygen utilization
Ø Act as α-adreno-receptor blockers and as serotonin and dopamine agonists
Ø Should be given early in the course of dementia
Ø Contraindicated in individuals who have previously shown hypersensitivity to the drug and history of psychosis
2. Cholinergic agents
Ø The cholinergic deficit hypothesis provides the most viable and consistent explanation for the memory impairment that occurs during Alzheimer’s but it does not account for all the clinical deficits that occur
Ø Comparisons between Alzheimer’s disease patients and age matched controls have demonstrated neuron losses in the nucleus basalis of Meynert, an area that is thought to provide cholinergic input and a major cholinergic pathway leading from the septum to hippocampus, a structure that is critical to normal memory function
Several pharmacological efforts to augment cholinergic activity have focused on:
- Increasing the acetyl choline synthesis and release
- Limiting the acetyl choline breakdown by inhibiting acetylcholine esterase and
- Directly stimulating the acetylcholine receptors
Agents such as choline and lecithin serve as precursors to acetylcholine
Lecithin(phosphatidyl choline) raises the plasma choline level
Examples of Cholinergic agents
• Donepezil
• Rivastigmine
• Physostigmine
• Tacrine
• Galantamine
• Cholinesterase inhibitors block the acetylcholinesterase(AChE) and increase the availability of the Ach in the synaptic cleft by limiting its breakdown
• AChE inhibitors have been used most extensively
• Administered both intravenously and orally
• Use of physostigmine is limited because of its short duration of action and adverse effects such as nausea, vomiting, diarrhoea, dizziness and headache
Tacrine
Ø Has a longer duration of action than physostigmine
Ø Elevates Ach levels in the cerebral cortex and has shown encouraging results
Ø Dose related benefits in cognitive function such as performance of recognition and attentional tasks and improved measures of quality life
Ø Nausea, vomiting, diarrhoea and anorexia are common dose related side effects
Ø High prevalance of abnormal liver function tests
Ø Should be used with caution in patients with GIT diseases, as it may increase gastric acid secretion and cardiovascular conditions
Ø Has a vagotonic effect on the pulse rate and can cause bradycardia with sick sinus syndrome (sinus node dysfunction)
Ø Metabolised by cytochrome P450 system
Ø Given 4 times a day in an empty stomach
Ø Therapy initiated at 10mg, four times a day for 6 weeks with transaminase levels measures every other week
Donepezil
Ø Piperidine cholinesterase inhibitor with specificity for inhibition of acetylcholinesterase
Ø Fewer peripheral side effects (such as nausea, vomiting, and diarrhoea) than with nonspecific cholinesterase inhibitors
Ø Beneficial in patients with moderate to severe AD
Ø Initiated at a 5-mg/day dose in the morning and titrated to 10 mg/day after 4 to 6 weeks if it is well tolerated
Ø Side effects nausea, vomiting and diarrhoea
Rivastigmine
• Has central activity at acetylcholinesterase and butyrylcholinesterase, but low activity at these sites in the periphery
• Should be initiated at a dose of 1.5 mg twice daily and titrated upward at a minimum of 2-week intervals to a maximum daily dose of 12 mg
• Not metabolized through the CYP450 enzyme system
• Cholinergic side effects are the most common adverse effects
Galantamine
• Allosteric potentiating ligand of human nicotinic acetylcholine receptors
• Weak competitive and reversible cholinesterase inhibitor in all areas of the body
• Increases the concentration and thereby action of acetylcholine in certain parts of the brain
• Modulate the nicotinic cholinergic receptors on cholinergic neurons to increase acetylcholine release
• It is recommended that a patient be continued on the maximum tolerated dosage, as accelerated cognitive deterioration has been seen with dosage reductions
• Should be initiated at 8 mg/day with dosage titration of 8 mg/day occurring at 4-week intervals
• Metabolized through the CYP450 2D6 and CYP450 3A4 pathways
3. Other Agents
Memantine
• NMDA-antagonist
• First in a novel class of Alzheimer’s disease medications acting on the glutamatergic system by blocking NMDA receptors
• Currently indicated for use in AD patients with moderate to severe illness
• Has 100% bioavailability regardless of administration with or without food. Protein binding is low
• Metabolism is minimal and is excreted through urine unchanged
• The half-life ranges from 60 to 100 h
• Should be initiated at 5 mg once a day and increased weekly by 5 mg a day to the effective dose of 10 mg twice daily
• Vitamin E and Selegiline
• Lipid lowering agents
• Gingo biloba
• Antiinflammatory agents- NSAIDS
GUIDELINES FOR CARE OF PATIENT WITH ALZHEIMER’S DISEASE
• Provide a calm,quiet environment
• Provide a consistent routine
• Perform adls at same time each day
• Avoid changes in routine or environment
• Reassure and explain frequently
• Do not argue with the patient
• Protect safety
• Patient at increased risk of accidents
• Eliminate caffeine from the diet
GUIDELINES FOR CARE OF THE CONFUSED PATIENT
• Provide activities to distract the patient from inappropriate behavior
• Maintain a regular routine
• Use patience and understanding
• Maintain a calm, quiet environment
• Use simple, clear words and sentences
• Give frequent praise and reassurance
• Use touch and other forms of nonverbal communication
• Use reality orientation
REALITY ORIENTATION
Helps the confused patient with reality by frequent reminders of:
• who he is
• where he is
• what time it is
Always call the patient by name and identify yourself
Repeat the date, time, and place to the patient throughout the day
GUIDELINES FOR CARE OF THE AGGRESSIVE/COMBATIVE PATIENT
• Do not respond in anger
• Leave and come back later if possible
• Be aware of warning signs of anger, such as muscle tension, restlessness, and pacing, crying, and loud speech
• Offer distractions
• Communicate and reassure
• Be aware of your nonverbal communication
• Sit down, you will appear less threatening
• Do not touch the patient without his permission
Summary
• The prevalence of Alzheimer’s disease (AD) increases with each decade of life and is more common in females.
• Neuritic plaques and neurofibrillary tangles are the pathologic hallmarks of AD.
• AD affects multiple areas of cognition and is characterized by a gradual onset with a slow progressive decline.
• Early initiation and continued, uninterrupted treatment provide the optimal cognitive benefit.
• Pharmacotherapy for AD focuses on impacting three domains: cognition, psychiatric symptoms, and activities of daily living.
• Cholinesterase inhibitors and memantine are used to treat cognitive symptoms of AD.
• Slow medication dosage titration with careful monitoring should be done to minimize the incidence of troubling adverse drug reactions.