Asthma

Objective
At the end of this PDF Notes, student will be able to
• Define Bronchial asthma
• Explain the pathophysiology of Bronchial asthma
• Describe the symptoms of Bronchial asthma
Asthma
• Disorder of the respiratory system that leads to episodic difficulty in breathing
• Chronic inflammatory disorder of the airways in which many cells and cellular elements play a role
• Mast Cells, Eosinophils, T Lymphocytes, Macrophages, Neutrophils , Epithelial Cells
Bronchial Asthma
ü Also called reversible airway obstruction
ü Clinical syndrome characterized by recurrent bouts of bronchospasm
ü Increased responsiveness of the tracheobronchial smooth muscles to various stimuli
ü Results in narrowing of the airway
ü Chronic inflammatory disorder with reversible airflow obstruction
ü Inflammation of bronchial wall mediated by eosinophils, mast cells & lymphocytes
ü Hyper-responsiveness of bronchi – narrow readily with stimuli
ü In late stages – irreversible
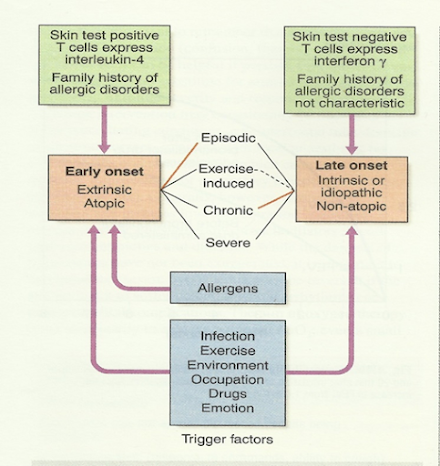
Etiology of Asthma
Extrinsic or allergic
ü History of `atopy` in childhood
ü Family history of allergies
ü Positive skin test
ü Raised IgE level
ü Below 30 years of age
ü Less prone to status asthmaticus
Intrinsic or idiosyncratic
ü No family history of allergy
ü Negative skin test
ü No rise in IgE level
ü Middle age onset
ü Prone to status asthmaticus
Triggers
Drugs
Aspirin, ibuprofen and other prostaglandin synthetase inhibitors, beta blockers
Foods
Nuts, fish, sea food, dairy products, food colouring
Other industrial chemicals
Wood or grain dust, cotton dust, cigarette etc
Miscellaneous
Cold, exercise, hyperventilation ,viral respiratory tract infections, emotion or stress
Pathophysiology of Asthma
Main features of asthma:
– Hypertrophy of bronchial smooth muscle
– Hyperplasia of epithelial cells
– Mucus gland hypertrophy
– Airway oedema
– Acute bronchoconstriction
– Impaired mucociliary clearance
• Early exposure to
– Allergens
– Viral infections
– Diet induced
• Early onset: Atopic
-Positive family history
-Readily form IgE to common allergens react with mast cells on surface & activate IgE – histamine release
-Many more mediators
v Changes in the airway
ü Epithelial shedding
ü Airway hyper-responsiveness
ü Microvascular leakage – exudate mucus plugging
ü Neuronal imbalance – bronchoconstriction
v IgE-antibody-mediated reaction on the surface of the mast cell leads to release of mast cell components
v Histamine – triggers rapid bronchoconstriction
v Eosinophils release LTC4 and PAF
v Epithelial damage and thick viscous mucus produced causing deterioration in lung function
v Epithelial damage
v Increases access of various irritants to the cholinergic receptors,
v Bronchoconstriction mediated by the parasympathetic nervous system
Signs and Symptoms of Asthma
• Persistent cough
• Dyspnoea – difficulty in breathing
• Wheezing – a high pitched noise due to turbulent airflow through a narrowed airway
• Tightness of chest
• Shortness of breath
• During attacks – fatigue, cyanosed, lethargic, confused, breathless, rapid breathing (> 30 breaths/minute)
Clinical Features of Asthma
• Episodic or chronic
• Triad of:
– Dyspnea (difficulty in breathing)
– Wheezing (additional sounds)
– Cough (persistent)
• Productive sputum
• Others
Tachycardia
Pulsus paradoxus
Sweating
Cyanosis, bradycardia in severe cases
Silent chest
Diagnosing Bronchial Asthma
Medical History and Physical Examination
Diagnosing asthma begins with a detailed medical history and physical examination. Your healthcare provider will ask about your symptoms, family history, and exposure to potential triggers.
Lung Function Tests
Lung function tests, such as spirometry and peak flow measurements, are essential for confirming the diagnosis. These tests assess how well your lungs are functioning and the degree of airway obstruction.
Management and Treatment
Medications
Asthma management often involves medications, including bronchodilators to relax the airways and corticosteroids to reduce inflammation. Inhalers are commonly used to deliver these drugs directly to the lungs.
Lifestyle Changes
In addition to medication, certain lifestyle changes can help control asthma. This may include identifying and avoiding triggers, maintaining a healthy weight, and staying physically active.
Living with Bronchial Asthma
Coping Strategies
Living with asthma requires adopting coping strategies to ensure a good quality of life. Education about the condition, a strong support system, and a written asthma action plan are all essential for managing asthma effectively.
SUMMARY
• Chronic inflammatory disorder with reversible airflow obstruction
• Inflammation of bronchial wall mediated by eosinophils, mast cells & lymphocytes
• IgE-antibody-mediated reaction
• Release of mast cell components which triggers rapid bronchoconstriction
• Persistent cough, recurrent episodes of difficulty in breathing associates with wheezing, chest tightness, shortness of breath, abnormal lung function are the common symptoms
Asthma PDF Notes
Frequently Asked Questions
frequently asked questions (FAQs) about bronchial asthma:
- Is bronchial asthma the same as chronic obstructive pulmonary disease (COPD)?No, bronchial asthma and COPD are distinct conditions with different underlying causes. While both involve breathing difficulties, the pathophysiology and management differ.
- Can asthma be outgrown, especially in children?Some children may experience a reduction in asthma symptoms as they grow older, but asthma can persist into adulthood. Regular follow-up with a healthcare provider is essential.
- Are all asthma triggers avoidable?While some triggers can be avoided, such as allergens, it may be challenging to avoid all environmental factors. Effective management involves both trigger avoidance and medication use.
- Can asthma attacks be fatal?In severe cases, asthma attacks can be life-threatening. It is crucial to have an asthma action plan and seek immediate medical attention if experiencing a severe attack.
- What role does genetics play in the development of asthma?Genetics can increase the risk of developing asthma, especially if there is a family history of the condition. However, environmental factors also play a significant role in its development.
- What are the potential complications of uncontrolled bronchial asthma?Uncontrolled asthma can lead to serious complications, including frequent asthma attacks, reduced lung function, and decreased quality of life. Long-term, it can result in chronic respiratory problems and, in severe cases, even life-threatening situations.
- Is bronchial asthma preventable?While asthma cannot be completely prevented, certain measures can reduce the risk of developing the condition. Avoiding exposure to tobacco smoke, allergens, and maintaining a healthy lifestyle can help lower the risk.
- Can bronchial asthma be managed without medication?In some cases, mild asthma can be managed with lifestyle changes and trigger avoidance alone. However, many asthma sufferers require medication to effectively control the condition and prevent symptoms.
- Are there different types of inhalers for asthma, and how do they work?Yes, there are various types of inhalers for asthma, including bronchodilators (relax the airways) and corticosteroids (reduce inflammation). Inhalers deliver medication directly to the lungs, providing rapid relief and minimizing side effects.
- Can people with asthma lead normal lives and engage in physical activities?
With proper asthma management, individuals with asthma can lead normal lives and engage in physical activities. In fact, regular exercise can improve lung function and overall well-being. It’s essential to consult with a healthcare provider to develop an asthma action plan that suits your lifestyle.