Hereditary Acquired Anaemia

Hereditary Acquired Anaemia
Objective
At the end of the PDF Notes, the students will be able to
• Explain hereditary acquired anaemia
• Describe the pathophysiology and clinical features of Hereditary Spherocytosis
• Explain the pathogenesis of hereditary disorders of red cell interior
• Explain haemoglobinopathies
Introduction
Anemia is a condition that arises when there is a reduced number of red blood cells or a decreased amount of hemoglobin in the blood. While anemia can be acquired due to various factors, hereditary acquired anemia is rooted in our genetic makeup, making it a unique and challenging condition to understand.
Hereditary Acquired Anemia
Hereditary acquired anemia is a subset of anemia that is inherited from our parents through genetic mutations. It encompasses a range of disorders, including Hereditary Spherocytosis.
• Hereditary haemolytic anaemias are usually the result of intracorpuscular defects.
• Classified into 2 groups:
1) Hereditary abnormalities of red cell membrane
2) Hereditary disorders of the interior of the red cells
A. Hereditary Abnormalities of Red Cell Membrane
3 important types of inherited red cell membrane defects:
1) Hereditary spherocytosis
2) Hereditary elliptocytosis (hereditary ovalocytosis)
3) Hereditary stomatocytosis.
Hereditary Spherocytosis Pathogenesis
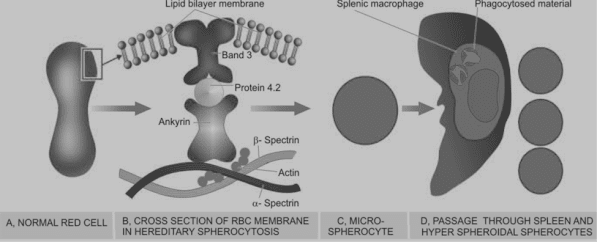
• The molecular abnormality in hereditary spherocytosis is a defect in proteins which anchor the lipid bilayer to the underlying cytoskeleton.
1) Spectrin deficiency: deficiency in the structural protein of the red cell membrane, spectrin
• Mutation in spectrin- α−spectrin- severe anaemia
• Mutation by β-spectrin results in mild Anaemia.
2) Ankyrin abnormality: defect in ankyrin, protein that binds protein 3 and spectrin
CLINICAL FEATURES
1. Anaemia is usually mild to moderate.
2. Splenomegaly is a constant feature
3. Jaundice occurs due to increased concentration of unconjugated (indirect) bilirubin in the plasma (also termed congenital haemolytic jaundice).
• 4. Pigment gallstones are
Hereditary Elliptocytosis (Hereditary Ovalocytosis)
• It is autosomal dominant disorder involving red cell membrane protein spectrin.
Hereditary Stomatocytosis
• Stomatocytes are cup-shaped RBCs having one surface concave and the other side as convex.
• This causes a central slit-like or mouth-like appearance of red cells.
• The underlying defect is in membrane protein stomatin
B. Hereditary Disorders of Red Cell Interior
• Inherited disorders involving the interior of the red blood cells are classified into 2 groups:
1. Red cell enzyme defects (Enzymopathies): These cause defective red cell metabolism involving 2 pathways
i) Defects in the hexose monophosphate shunt
ii) Defects in the Embden-Meyerhof (glycolytic) pathway
2. Disorders of haemoglobin (haemoglobinopathies):
These are divided into 2 subgroups:
i) Structurally abnormal haemoglobin: Examples are sickle syndromes and other haemoglobinopathies.
ii) Reduced globin chain synthesis: Common examples are various types of thalassaemias.
Red Cell Enzyme Defects (Enzymopathies) G6PD Deficiency
• Defects in hexose monophosphate shunt- G6PD deficiency
• G6PD gene is located on the X chromosome – affecting males
PATHOGENESIS
PK Deficiency
• Pyruvate kinase (PK) deficiency is the only significant enzymopathy of the Embden-Meyerhof glycolytic pathway.
• The disorder is inherited as an autosomal recessive pattern. Heterozygote state – asymptomatic
• Homozygous individual presents during early childhood with anaemia, jaundice and splenomegaly.
Haemoglobinopathies
• Haemoglobin in RBCs may be abnormally synthesised due to inherited defects. These disorders may be of two types:
1) Qualitative disorders in which there is structural abnormality in synthesis of haemoglobin e.g. sickle cell syndrome, other haemoglobinopathies.
2) Quantitative disorders in which there quantitatively decreased globin chain synthesis of haemoglobin e.g. thalassaemias.
Summary
Ø Important types of inherited red cell membrane defects:
1) Hereditary spherocytosis
2) Hereditary elliptocytosis (hereditary ovalocytosis)
3) Hereditary stomatocytosis
• Hereditary spherocytosis is a common type of hereditary haemolytic anaemia- defect in proteins which anchor the lipid bilayer to the underlying cytoskeleton
• Hereditary elliptocytosis or hereditary ovalocytosis is another autosomal dominant disorder involving red cell membrane protein spectrin
• Hererditary stomatocytes are swollen red cells (overhydrated red cells) due to increased permeability to sodium and potassium. The affected patients have mild anaemia and splenomegaly.
• Inherited disorders involving the interior of the red blood cells are classified into 2 groups: Red cell enzyme defects (Enzymopathies) and disorders of haemoglobin (haemoglobinopathies)
FAQs on Hereditary Acquired Anemia
Q1: Are hereditary acquired anemia and acquired anemia the same?
No, hereditary acquired anemia is a subset of anemia that is inherited through genetic mutations, while acquired anemia can be caused by factors like nutrition, illness, or medication.
Q2: How is Hereditary Spherocytosis diagnosed?
Diagnosis typically involves blood tests, including a complete blood count (CBC), and sometimes genetic testing to identify specific mutations.
Q3: Can hereditary acquired anemia be cured?
While there is no cure, many treatment options are available to manage the condition and improve the patient’s quality of life.
Q4: What are the long-term complications of hemoglobinopathies?
Hemoglobinopathies can lead to various complications, including organ damage, strokes, and frequent pain episodes.
Q5: Is genetic counseling recommended for families with a history of hereditary acquired anemia?
Yes, genetic counseling can provide valuable insights into the risks of passing on the condition to offspring and help individuals make informed family planning decisions.