Dispensing Errors
Learning Objectives
At the end of this lecture, student will be able to:
• List the prescription errors
• Indicate the remedial measures to avoid prescription
errors
• List the methods available for pricing of prescription
• Explain the methods involved in pricing of prescription
Dispensing / Medication Errors
• Defined as any error in the prescribing, dispensing, or administration of a drug, irrespective of whether such errors lead to adverse consequences or not
• Any preventable event
• Inappropriate medication use or patient harm
• In the control of the health care professional, patient or consumer
Most Prevalent Dispensing Errors
Types of Dispensing Errors
• Commission versus omission
• Mistake versus slip
• Potential versus actual
Errors of Omission
• Failure to counsel the patient
• Failure to screen for interactions and contraindications
Errors of Commission
• Miscalculation of a dose
• Dispensing the incorrect medication, dosage strength, or dosage form
Mistakes and slips
Mistake
• Do things intentionally but actions are incorrect because
of a knowledge or judgment deficit
• Example: dose prescribed that exceeds maximum safe limit
Slip
• Do things unintentionally incorrect because of an attention
deficit
• Example: dispense chlorpromazine when prescription was clearly written for chlorpropamide
Types of Dispensing Errors
1. Dosage errors
2. Time errors
3. Unauthorized errors
4. Technique errors
5. Administration route errors
6. Extradoses doses
7. Prescription errors
8. Omissions
9. Wrong patient
10. Presentation error
Can you read this???
Neither can we!!!
DISPENSING ERROR
• From the receipt of the prescription in the pharmacy to
the supply of a dispensed me to the patient.
• This occurs primarily with drugs that have a similar name
or appearance.
• Example: Lasix® (Frusemide) and Losec® (Omeprazole)
• Other potential dispensing errors include wrong dose, wrong drug, wrong administration or wrong patient
Assessing Prescriptions
• Clarify illegible handwriting, nonstandard abbreviations,
or incomplete information
• Analyze patient’s profile
• Review drug interactions & allergies
• Verify appropriateness of medication and dosage
• Consider computer alerts
• Highlight unusual dosage form or strength
Illegible handwriting
Humulin “Log” ordered
instead of Humulin-L (Lente).
Nurse thought
Humalog” was to be given
Unasyn or Vancomycin?
Appropriateness of medication and dosage
• Check if the drug is right for the patient (Men/ Women)
• Check if the dose is in accordance with weight, age, body surface area, existing health conditions…..
• Check if the dosage form is in accordance with age
Dosage errors
• Mathematical errors and decimal point misplacement are common causes of errors, especially in conversions between micrograms and milligrams
• Oral liquid medications can be dispensed improperly
because of misunderstandings with reading and labeling
• Always use leading zeros for decimal points. The order should have read: Digoxin 0.5 mg
• Medications administered in doses greater or smaller than
what had been prescribed
Example:
Prescription for 25mg of Captopril and a 50mg dose was administered
Time Errors
• Medication administered to patient early or late than the time which had been prescribed.
Examples:
Prescription for Vancomycin at 6 pm and administered at
7:20pm or Enalapril at 10 am and administered at 8.30am.
Unauthorized errors
• Administering medication that has not been prescribed by
the physician.
Examples:
Administering Amoxicillin instead of Amoxicillin combined
with Clavulanate
Technique Errors
• Medication incorrectly formulated or manipulated before
administering or
Examples:
Not measuring doses appropriately, to administer iron
sulfate alter meals.
Not verifying the systemic arterial blood pressure before
administering hypertensive mediation
Administration Route Errors
• Administering medications using a route different than
prescribed.
Examples:
Prescription for intramuscularly administration and
administered intravenously (E.g. Insulin)
Prescription for sublingual administration and administered
orally (E.g. Nitroglycerin)
• Patient took Rogaine internally and applied Viagra
externally
Administration errors
• Discrepancy occurs between the drug received by the
patient and the drug therapy intended by the prescriber.
• Errors of omission – the drug is not administered
• Incorrect administration technique and the administration
of incorrec or expired preparations
• Deliberate violation of guidelines
Causes of administration errors
• Lack of perceived risk
• Poor role models
• Lack of available technology
• Lack of knowledge of the preparation or administration procedures
• Complex design of equipment.
Contributing factors to drug administration errors
• Failure to check the patient’s identity prior to
administration
• Environmental factors such a noise, interruptions, poor lighting
• Wrong calculation to determine the correct dose
Approaches to reduce drug administration errors include:
• Checking the patient’s identity
• Ensuring that dosage calculations are checked
independently by another health care professional before the drug is administered
• Ensuring that the prescription, drug, and patient are in
the same place in order that they may be checked against one another
• Ensuring the medication is given at the correct time
• Minimizing interruptions during drug rounds
Action to be taken when error occurs
• The client safety becomes the top priority
• The nurse assesses and examines the client’s condition and notifies the physician of the incident as soon as possible.
• Once the client is stable the nurse reports the incident
to the appropriate person in the institution like nursing supervisor or nursing manager.
• The nurse is also responsible for reporting the incident.
An incident report usually must be filed within 24hours of an incident.
• The report includes client identifying information, the
location and time of the incident, an accurate factual description of what occurred and what was done, the signature of the nurse involved
• The incident report is not a permanent part of the medical
record and should not be referred to in the record. This is to legally protect the health care professional and institution
• The institution use incident report to track incident
pattern and to initiate quality, improvement programs as needed.
• It is good risk management to report all medication error
including mistakes that do not cause obvious or immediate harm or near misses.
Extradoses errors
• Administering more or extra dose than what has been prescribed.
• Prescribing which has been suspended in prescription.
Example:
Administering Captopril that later was suspended in the prescription.
Prescription Errors
• Incorrect selection of the medication, dosage administration route, use instructions by physician orally and not registering a verbal prescription.
Example:
Prescribing Omeprazole for 8 pm. when it should be administered at 6pm before dinner.
Look alike drugs
• The drug Hydralazine, on the left, is used to treat high
blood pressure, while Hydroxyzine is used to treat itching or allergies. Taking blood pressure medicine unnecessarily could cause someone to faint, whereas taking an allergy medicine instead of Hydralazine would leave high blood pressure untreated and could lead to stroke.
Omissions
• Failure to counsel the patient
• Failure to screen for interactions and contraindications
Example:
The professional prepared the aerosol with saline at 0.9%
and did not add the Imatropium bromide that had also been prescribed.
Wrong Patient
• Administering the medication to a wrong patient
Example:
Phenytoin was prescribed to patient A but was administered
to patient C
Presentation Error
• Administering medication in a way different from what had been prescribed
Example:
Furosemide tablets were administered instead of ampoule
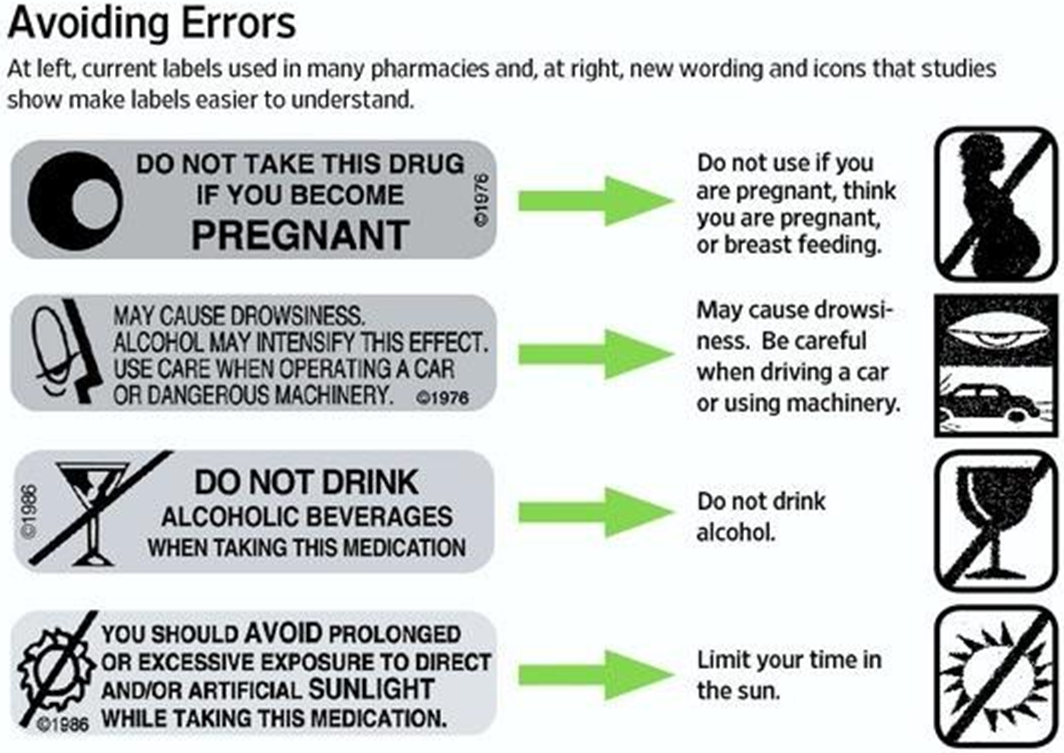
Dispensing errors caused by poor labeling
• Pharmacy computer-generated labeling and production of
medication administration records should be optimized
• Nonessential information should be excluded from labels
and reports
• Lack of a real understanding of the patient information in
the leaflet provided, results in poor adherence to the medication requirements
Risk factors for prescribing/ dispensing errors
Work environment
Workload
Communication within the team
Physical and mental well being
Lack of knowledge
Organizational factors such as inadequate training
Low perceived importance of prescribing
An absence of self-awareness of errors
Dispensing Errors: Common Causes
• Work environment
– Workload
– Distractions
– Work area
• Use of outdated or incorrect references
Dispensing Errors: Improving Workload
• Ensure adequate staffing levels
• Eliminate dispensing time limits (quotas)
• Examples of limiting workload
– Dispense ≤150 prescriptions per pharmacist per day
– Require rest breaks every 2–3 hours
– Brief warm-up period before restarting work tasks
– Require 30-minute meal breaks
Dispensing Errors: Combating Distractions
• Phones and fax machines
• Prohibit distractions during critical prescription-filling
functions
• Centralized filling operations
• Train support personnel to answer the telephone
Dispensing Errors in the Work Area
• Clutter (return used containers immediately)
– Ensure adequate space
– Store products with label facing forward
– Choose high-use items on the basis of safety as well as
convenience, use original containers
• Lighting
• Heat, humidity
• Noise (TV, radio)
• Labels on ingredient containers and shelves
• Separate by route of administration (external/ internal/ injectable, etc.)
• Use auxiliary labels for externals
– Amoxicillin oral suspension for ear infection thought by parents to be drops administered in child’s ear
• Review published safety alerts for look-alike/ sound-
alike drugs and frequent dispensing errors
Cognitive and Social Factors
• Use of high-intensity task lights and magnification
• Use of a device to hold prescriptions/orders at eye level
• Posting alerts in strategic locations with error-prone
products
• Use of exaggerated, unconventional type fonts to enhance reading of drug names
Well-Designed Drug Storage
• Adequate space
• Label facing forward
• Agents for external use should never be stored with oral medications
• Separate by route of administration
• Mark and/or isolate high-alert drugs
• Separate sound-alike/look-alike drugs
Errors Related to Information about the Drug or Patient
• Misleading or erroneous references
• Ambiguity in handwritten and typed documents
• Computerized prescribing
• Wrong patient errors
• Errors in dosage
Computerized Prescribing Errors
• Computerized prescriber order entry (CPOE) improves communication and reduces some types of errors
• However, this technology may have its own pitfalls:
– Lower case L may look like the numeral 1
– Letter O may look like the numeral 0 (zero)
– Letter Z and the numeral 2 may be misread
– Wrong patient or wrong drug chosen from list
Computerized Alerts
• Computer systems can be configured to flash maximum dose alerts and other safety alerts
• Upgrades are necessary and usually available from software vendors
Optimal Capabilities of Pharmacy Computer Software to Prevent Dispensing Errors
• Dose limits
• Allergic reactions
• Cross-allergies
• Duplication of drug ingredients
• Drug interactions
• Contraindicated drugs or drugs that need dosage
modifications
Outpatient Label Content
• Patient name
• Medication name
• Dosage strength
• Dosage form
• Quantity
• Directions for use
• Number of refills
• Prescriber name
• Purpose of medication
Manual rechecking
• Independent double checks before dispensing
– Original prescription order, label, and medication
container should be kept together throughout the dispensing process
– Pharmacist must check all of technician’s work
• Self-checking by a lone practitioner may be safer if:
– Switching hands when rereading the label
– Delay of self-checking
– Recalculating using a different process
• Compounded products can be checked before dispensing
utilizing new qualitative and quantitative analysis techniques
• Use of standardized concentrations of frequently used
formulations reduces errors
Dispensing Errors Caused by Poor Patient Education
• Failure to adequately educate patients
• Lack of pharmacist involvement in direct patient education
• Failure to provide patients with understandable written
instructions
• Lack of involving patients in check systems
• Not listening to patients when therapy is questioned or
concerns are expressed
Counseling Patients
• A majority of dispensing errors can be discovered during
patient counseling and corrected before the patient leaves the pharmacy
Good Patient Education
• Inform patients of drug names, purpose, dose, side
effects, and management methods
• Suggest readings for patient
• Inform patient about right to ask questions and expect
answers
• Listen to what patient is saying and provide follow-up
Approaches for reducing prescribing errors
• Electronic prescribing may help to reduce the risk of
prescribing errors resulting from illegible handwriting
• Computerized physician order entry systems eliminate the
need for transcription of orders by nursing staff
Steps to be taken in preventing medication error
•Follow the rights of medication administration
•Right patient
•Right drug
•Right dose
•Right time
•Right route
•Right recording
•Right assessment
•Right education
•Right evaluation
•Right to refuse medication
• Be sure to read labels at least 3 times, before during after
administration of the drug.
• Prepare the medicine in a well-lighted room.
• Check the expiry date of the drug before administration.
• Be aware about ambiguous orders or drug names and
numerical and Consult doctor if any doubt.
• Be alert to usually large dosage or excessive increase in
dosage ordered.
• When in doubt, check order with prescriber, pharmacist, literature.
• Double check all calculation, even simple calculation
• Do not allow any other activity to interrupt your administration of medication to a client
• Routinely refer to drug interaction charts or drug
reference source and commit common interactive drugs to memory
• Do not use any unstandard abbreviation and symbols,
question if any one use
• Read the leaflet of the drug carefully when giving new drug
first time
• Do not make assumptions of illegible orders
• Do not accept incomplete orders and telephonic or verbal
orders
• Double check with a patient who has allergies about all
new drugs as they are added in treatment plan
• Question a drug form used in unfamiliar way
• Document all medication as soon as they are given
• When you have made an error reflect on what went wrong,
ask how you could have prevented the error
• Evaluate the context for any medication error to determine
if nurses have the necessary resources for safe medication administration
• When repeated medication error occurs within a work area,
identify and analyze the factors that may have caused the errors and take corrective action
• Attend in-service program that focus on the drug you
commonly administer.
Pricing the Prescription
• The Pharmacist should effectively manage the financial aspects of his practice.
The cost applied to the prescription should cover the
following:
• Cost of ingredients, including the container and label.
• The time devoted by the pharmacist and other operational
cost of the department.
• Cost of inventory maintenance and other operational cost
of the department.
• Providing reasonable margin of profit on investment.
Pricing Schedules
• The most common methods of pricing are:
• % mark up
• % mark up + minimum fee
• Professional fee
• Summation
% mark up
Dispensing price = Cost of ingredients + (cost of ingredients X % markup)
Eg. If the ingredients in a prescription cost Rs. 100 and he
wishes to apply 40% mark up on the cost, he would add Rs 40 to the cost of the ingredients and the dispensing price would be Rs. 140.
[100 + (40 % of 100)]
= 100+40=140
% mark up + minimum fee
Dispensing cost = Cost of ingredients + (cost of ingredients X % markup) + minimum fee
• In this method, a minimum fee is added to the cost of ingredients including a percentage mark up.
• The minimum – cost of the container, label, overhead and professional services.
• The minimum fee covers overhead expenses.
• Overhead expenses – rent, heat, refrigeration, electricity, taxes, insurance, depreciation in equipment, deterioration of drugs, interest on investment, delivery service
• Average overhead cost per prescription- total overhead expenses of the prescription department divided by the total prescription dispensed over a specific period of time.
Professional Fee
Dispensing price = Cost of ingredients + Professional fee
• The professional fee includes all the dispensing cost and
professional remuneration.
• A pharmacy may determine its professional fee by using
cost analysis method.
Summation
Dispensing price = Sum of all costs + profit
• Each component cost is determined individually for each
prescription and totaled. This equals the break-even point. To this a profit is added to obtain the dispensing price.
• Economical but complicated, cumbersome and time consuming.
Summary
• Prescription Errors and Its Types.
1. Dosage errors
2. Time errors
3. Unauthorized errors
4. Technique errors
5. Administration route errors
6. Extradoses doses
7. Prescription errors
8. Omissions
9. Wrong patient
10. Presentation error
• Pricing Schedules
1. % mark up
2. % mark up + minimum fee
3. Professional fee
4. Summation