The cardiovascular system
Objectives
At the end of this
lecture, student will be able to
• Explain the location of the heart
• List the chambers, great vessels and valves of the heart
• Describe the structure and functions of the pericardium,
heart wall, chambers
• Describe the structure and functions of heart chambers and
great vessels
• Outline the blood flow through the chambers of the heart
• Explain the operation of heart valves
• Explain pulmonary and systemic circulation
• Explain conduction system of heart
• Explain the pressure and volume changes of cardiac cycle
• Explain cardiac output and stroke volume
• Outline the structure and function of:
– Arteries
– Arterioles
– Capillaries
– Venules
– Veins
• Explain the events of ECG
• Define blood pressure
• Describe the factors affecting BP
• Explain echocardiogram
• Explain the regulation of BP
• Point out and summarize the common disorders of
cardiovascular system
Content
• Anatomy of heart
• Heart chambers
• Heart valves
• Operation of heart valves
• Pulmonary and systemic circulation
• Conduction system
• Cardiac cycle
• Innervation of heart
• Structure of blood vessels
• ECG
• Blood pressure
• Factors affecting blood pressure
• Echocardiogram
• Regulation of blood pressure
• Disorders of cardiovascular system
Introduction
to Cardiovascular System
• Center of the cardiovascular system – the heart
• Connects to blood vessels that transport blood
• To accomplish this, heart beats about 100,000 times every
day, (35 million beats in a year)
• Cardiology – Study of the normal heart and the diseases
associated
Cardiovascular
System
• Arteries
– carry blood away from the heart
– carry blood high in oxygen (except for the pulmonary arteries)
• Veins
– Veins carry blood back to the heart
– carry blood low in oxygen (except for the pulmonary veins)
• The great vessels
– Arteries and veins entering and leaving the heart
Characteristics
and Functions of the Heart
• Ensures the unidirectional flow of blood
• Backflow of blood is prevented by valves within the heart
• Acts like two independent, side-by-side pumps
– One directs blood to the lungs for gas exchange
– The other directs blood to body tissues for nutrient
delivery
• Develops blood pressure through alternate cycles of heart
wall contraction and relaxation
Anatomy of
the Heart
• Relatively small, conical organ
• Size of a person clenched fist
• Weighs about 250 to 350 grams
• Located left of the body midline
• Posterior to the sternum in the middle mediastinum
• Right side – Located anteriorly
• Left side – Located posteriorly
• Base: Formed
primarily by the left atrium
• Apex – The
inferior & conical end
• It projects slightly anteroinferiorly toward the left side
of the body
The Heart
Pericardium
• Fibrous, serous sac
• Confines the heart
• Allows sufficient of movement for vigorous and rapid
contraction
• Restricts heart movements
• Prevents the heart
from overfilling
• Between the parietal & visceral layers
– Thin film of lubricating serous fluid
• Outer Portion
– Tough, dense connective tissue
– Called the fibrous pericardium
– Attached to the sternum & diaphragm
– Prevents overstretching, provid protection
– Anchors the heart in the mediastinum
• Inner Portion
– Thin, double-layered serous membrane
– Called the serous pericardium
• Parietal layer – Fused to the fibrous pericardium
• Visceral layer (Epicardium – Adheres tightly to the
surface of the heart)
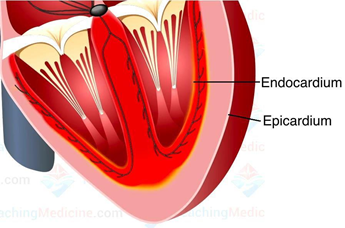
Heart Wall
Structure
Three distinctive layers:
– External epicardium
– Middle myocardium
– Internal endocardium
• Outer layer
• Simple squamous epithelium underlined by fat
• Age – More fat is deposited in the epicardium – thicker
and fattier
• Gives slippery texture to the outmost surface of the heart
• Myocardium
– Middle layer of the heart wall
– Composed chiefly of cardiac muscle tissue
– Makes up about 95% of the heart
– Responsible for its pumping action
• Endocardium
– Thin layer of endothelium
– Provides a smooth lining for the chambers of the heart
– Covers the valves of the heart
– Minimizes surface friction as blood passes through the
heart and blood vessels
Cardiac Muscle Tissue
• Fiber
Characteristics
– Short, branched fibers
– One or two central nuclei
– Numerous mitochondria for ATP supply
– Striated, with extensive capillary networks
• Intercalated discs
– Specialized cell–cell contacts
– Contain gap junctions
– Contain desmosomes
External
Anatomy of the Heart
• Chambers:
– Four hollow chambers:
• Two smaller atria
• Two larger ventricles
Atria
• Thin-walled, located superiorly
Auricle:
– Anterior part of each atrium is a wrinkled, flap like
extension
– Slightly increases the capacity of an atrium
Receive blood through
both circulatory circuits
• Right atrium receives blood from the systemic circuit
• Left atrium receives blood from the pulmonary circuit
• Blood that enters an atrium is passed to the ventricle on
the same side of the heart
Ventricles
– The inferior chambers
– Two large arteries, the pulmonary trunk and the aorta exit
the heart at the basal surface
– The pulmonary trunk carries blood from the right ventricle
into the pulmonary circuit
– The aorta conducts blood from the left ventricle into the
systemic circuits
• Atria are separated from the ventricles externally by
coronary sulcus (or atrioventricular sulcus)
• Extends around the circumference of the heart
• The anterior interventricular sulcus and the posterior interventricular
sulcus are located between the left and right ventricles
• These sulci extend inferiorly from the coronary sulcus
toward the heart apex
Chambers of
the Heart and Valves
Right
Atrium
• The posterior wall is smooth
• The anterior wall is rough:
– Due to the presence of muscular ridges called pectinate
muscles
– Extend into the auricle
• Contains fossa ovalis
• Interatrial septum
– Thin partition between the right and left atrium
Left Atrium
• Same thickness as the right atrium
• Forms most of the base of the heart
• Smooth posterior wall
• Pectinate muscles are confined to the auricle of the left
atrium
Right
Ventricle
• The right ventricle is about 4–5 mm in average thickness
• Interventricular septum: Separates the ventricles
• The inside of the
right ventricle
– Contains a series of ridges formed by raised bundles of
cardiac muscle fibers called trabeculae carneae
• Chordae tendineae:
– Tendon like cords- connected to cone shaped trabeculae carneae
called papillary muscles
– The cusps of the tricuspid valve are connected to the
chordae tendineae
Left
Ventricle
• Thickest chamber of the heart
• Forms the apex of the heart
• Like the right ventricle, the left ventricle contains:
– Trabeculae carneae
– Chordae tendinae – Anchor the cusps of the bicuspid valve
to papillary muscles
Heart
Valves
• As each chamber of the heart contracts – Pushes a volume
of blood into a ventricle or into an artery
• Valves open and close in response to pressure changes as
the heart contracts and relaxes
• Each of the four valves helps ensure the oneway flow of
blood
AV Valves
• Bicuspid – Left
• Tricuspid – Right
Semilunar Valves
• Pulmonary valve
• Aortic Valve
Operation
of AV Valves
(a) AV
valves open, atrial pressure greater then ventricular pressure
1. Blood returning to the heart fills atria, putting
pressure against atrioventricular valves; atrioventricular valves are force to
open
2. As ventricles fill, atrioventricular valves flaps hang
limply into ventricles.
3. Atria contract, forcing additional blood into ventricles.
(b) AV
valves closed, atrial pressure less then ventricular pressure
1. Ventricles contract, forcing blood against
atrioventrcular valve cusps.
2. Atrioventrcular valve closed
3. Pipillary muscles contract and chordae tendineae tighten,
preventing valve flaps from everting into atria
Operation
of Semilunar Valves
(a) Semilunar
valves open
As ventricles contract and intraventricular pressure rises,
blood is pushed up against semilunar valves, forcing them open.
(b) Semilunar
valves close
As ventricles relax and intraventricular pressure falls,
blood flow back from arteries, falling the cusps of semilunar valves, forcing
them to close.
Pulmonary
and Systemic Circulation
• The heart pumps blood into two closed circuits with each
beat
– Systemic circulation
– Pulmonary circulation
• The left side of the heart
– Pump for systemic circulation
– Receives bright red, oxygen reach blood from the lungs
• The right side of the heart
– Pump for pulmonary circulation
– Receives all the dark red, deoxygenated blood returning
from systemic circulation
Pulmonary
and Systemic Circuits
The Systemic Circuit
• Consists of the chambers on the left side of the heart
• All the other named blood vessels
• Carries blood to all the peripheral organs of the body and
tissues
The pulmonary circuit
• Consists of the chambers on the right side of the heart
• Pulmonary arteries and veins
– conveys blood to the lungs via pulmonary arteries
– To reduce CO2 and replenish O2 levels in the blood
– Blood returns to the heart in pulmonary veins
Pulmonary and
Systemic Circuits
Step 1. Oxygenated blood from the left side of the heart –
Pumped into the aorta
Step 2. Then into smaller systemic arteries. Gas exchange in
tissues occurs from capillaries
Step 3. Systemic veins then carry deoxygenated blood and
waste products
Step 4. Most veins merge and drain into the superior and
inferior vena cavae
Step 5. Drain blood into the right atrium
Step 6. Blood enters the pulmonary circuit (cycle is
repeated)
Coronary
Circulation
• The coronary
arteries
– Branch from the ascending aorta
– Encircle the heart
• While heart
contracts
– Little blood flows in the coronary arteries because they
are squeezed shut
• When heart relaxes
– The high pressure of blood in the aorta propels blood
through the coronary arteries
– Into capillaries
– Then into coronary veins
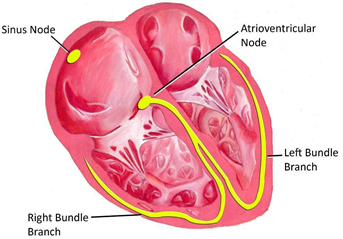
The
Conduction System
Autorhythmic fibers
(Self-excitable):
– Network of specialized cardiac muscle fibers
– The source of electrical activity
• Repeatedly generate AP
• AP trigger heart contractions
• Carry out 2 important functions:
– Act as a pacemaker
– Form the conduction system
Components of
the Conduction System
• Sinoatrial (SA)
node (pacemaker)
• Atrioventricular (AV) node
• Atrioventricular (AV) bundle (bundle of His)
• Bundle branches
• Purkinje fibers
Sinoatrial (SA) node
(pacemaker)
• Act as the pacemaker
• Located in the posterior wall of the right atrium
• Adjacent to the entrance of the superior vena cava
Atrioventricular (AV)
node
• Internodal conduction pathway
• Located in the floor of the right atrium between the right
AV valve and the coronary sinus
Atrioventricular (AV)
bundle (bundle of His)
• From the AV node to AV bundle
• Extends into the interventricular septum
• Then divides into one right and two left bundle branches
• Conduct the impulse to conduction fibers called Purkinje
fibers in the heart apex
Purkinje fibers
• Muscle impulse conduction – Extremely rapid
• Impulse spreads immediately throughout the ventricular
myocardium
Role of
Conduction System
Cardiac cycle
• Series of events that occur in single heart beat
• A cardiac cycle consists of:
– Systole (contraction)
– Diastole (relaxation) of both atria & ventricles
• With an average heartbeat of 75 beats/min, a complete
cardiac cycle requires 0.8 seconds
Cardiac
output
• The volume of blood ejected from the left ventricle (or
the right ventricle) into the aorta (or pulmonary trunk) each minute
Cardiac reserve
• Difference between your maximum heart rate and resting
heart rate
Factors regulate
stroke volume
• Preload
– The degree of stretch on the heart before it contracts
• Contractility
The forcefulness of contraction of individual ventricular
muscle fibers
• Afterload
– The pressure that must be exceeded before ejection of
blood from the ventricles
Auscultation
• The act of listening to sounds within the body
• Done with a stethoscope
• From blood turbulence caused by the closing of the heart
valves
• Smoothly filling blood is silent
Heart Sounds
• S1-lubb-closure of AV valve
• S2-dupp- closure of SL valve
• S3-rapid ventricular filling
• S4 -atrial systole
Innervation
of the Heart
• Innervated by ANS
• Consists of both sympathetic and parasympathetic
components
• Rich innervation to SA and AV nodes, but also to
myocardial cells
• Parasympathetic
innervation
– Via right and left vagus nerves
– Decreases HR & FOC
• Sympathetic
innervation
– Via cardiac nerves
– Increases the rate and the FOC
Nervous
Control of the Heart
Basic
Structure of a Blood Vessel
Blood
vessels
• Large arteries – Elastic (conducting) arteries
• Medium-sized arteries – Muscular (distributing) arteries
• Arterioles – Small arteries that deliver blood to
capillaries
• Through constriction and dilation, arterioles assume a key
role:
• Un-regulating blood flow
• In altering arterial blood pressure
Veins
• Venules – Small vessels that continue from capillaries
• Merge to form veins
• Veins – Consist of the same three tunics as arteries
• Valves – Prevent backflow of blood
• Systemic veins are collectively called blood reservoirs
• They hold a large volume of blood
Capillaries
• Microscopic blood vessels
• Materials are exchanged between blood and tissue cells
• Some capillaries are continuous, and others are
fenestrated
• Branch to form an extensive network throughout a tissue
Anastomose
• The distal ends of two or more vessels unite
• An alternative blood route from an anastomosis – collateral
circulation
• Arteries that do not anastomose are called end arteries
Electrocardiogram
(ECG)
• AP propagate through the heart
• Generate electrical currents
• Can be detected at the surface of the body
• An electrocardiogram (ECG or EKG):
– Recording of electrical signals of the heart
• Electrodes – Positioned on the arms and legs (limb leads)
and at six positions on the chest (chest leads) to record
• Amplifies the heart’s electrical signals
• Each electrode records slightly different electrical
activity
• Position relative to the heart
Significance of ECG
• By comparing these records with one another and with
normal records, it is possible to determine–:
(1) If the conducting pathway is abnormal
(2) If the heart is enlarged
(3) If certain regions of the heart are damaged
(4) The cause of chest pain
Normal ECG
• Consists of:
– P wave
– QRS complex
– T wave
• P wave: Atrial
depolarization
• QRS complex:
Onset of ventricular depolarization
• T wave:
Ventricular repolarization
• The P-Q interval:
Beginning of atrial excitation to the beginning of ventricular excitation
• The S-T segment: Represents
the time when ventricular contractile fibers are fully depolarized
Blood
Pressure
• Hydrostatic pressure exerted by blood on the walls of a
blood vessel
• Contraction of the ventricles generates blood pressure
• BP is determined by
– Cardiac output
– Blood volume
– Vascular resistance
• Systolic BP-
Highest pressure attained in arteries during systole
• Diastolic BP-
Lowest arterial pressure during diastole
Mean
Arterial Pressure (MAP)
• The average blood pressure in arteries
• Roughly one-third of the way between the diastolic and
systolic pressures
• It can be estimated as follows:
MAP = diastolic BP + 1/3 (systolic BP – diastolic BP)
Eg. Thus, in a person whose BP is 110/70 mmHg,
[70 + 1/3(110 – 70)]= MAP is about 83 mmHg
Factors
Affecting BP
Vascular resistance
• Opposition to blood flow due to friction between blood and
the walls of blood vessels
• It depends on
– Size of the blood vessel lumen, Blood viscosity &
Total blood vessel length
• SVR or TPR: Refers to all the vascular resistances offered
by systemic blood vessels
• Most resistance- In the smallest vessels
Velocity of Blood
Flow
Venous Return (VR)
Blood from
the Lower Body Back To the Heart
• Two pump blood from the lower body back to the heart:
(1)The respiratory pump – based on alternating compression
and decompression of veins
(2) The skeletal muscle pump
Echocardiogram
• Uses ultrasound waves to examine the heart
• Non-invasive test
• To diagnose – abnormalities of the heart
Significance
• Size and shape of the heart
• Pumping efficiency of the heart
• Valve abnormalities
• Other – Detect the presence of fluid around the heart;
blood clots, or masses inside the heart; and abnormal holes between heart
chambers
Control of
Blood Pressure
• The cardiovascular (CV) center:
– Group of neurons in the medulla oblongata
– Regulates HR, contractility, and blood vessel diameter
– Receives input from higher brain regions and sensory
receptors (Baroreceptors and Chemoreceptors)
– Output from the cardiovascular center flows along
sympathetic and parasympathetic axons
Neural
Regulation of BP
• Sympathetic impulses
– Propagated along cardio – accelerator nerves
– Increase HR and FOC
• Parasympathetic impulses
– Propagated along vagus nerves
– Decrease HR
• Baroreceptors –
Monitor blood pressure
• Chemoreceptors –
Monitor blood levels of O2 &CO2 and H+ ions
• The carotid sinus reflex – Helps regulate blood pressure in
the brain
• The aortic reflex regulates general systemic blood pressure
Hormonal
Regulation of BP
• Hormones that help regulate blood pressure are:
• epinephrine
• nor-epinephrine
• ADH (vasopressin)
• angiotensin II
• ANP
Autoregulation
• Refers to local, automatic adjustments of blood flow in a
given region to meet a particular tissue’s need
• O2 level is the principal stimulus for autoregulations
Arrhythmia
or dysrhythmia
• Refers to an abnormal rhythm as a result of a defect in
the conduction system of the heart
• The heart may beat irregularly, too quickly, or too slowly
• Symptoms include
– Chest pain
– Shortness of breath
– Lightheadedness
– Dizziness and fainting
Hypertension
• Persistently high blood pressure
• Most common disorder affecting the heart and blood vessels
• Major cause of heart failure, kidney disease, and stroke
Hypotension
• Low blood pressure
• Commonly used to describe an acute drop in BP – excessive
blood loss
• Symptoms include
– Dizziness
Weakness
Lightheadedness
Syncope
Nausea
Transient ischemic attacks
Disturbed speech
Vision change
Angina pectoris
Arteriosclerosis
– Group of diseases
– Thickening of the walls of arteries
– Loss of elasticity
Atherosclerosis
– One form of arteriosclerosis
– A progressive disease
– Characterized by the formation of lesions –
atherosclerotic plaques
Myocardial
infarction (Heart attack)
• Happens when blood stops flowing properly to part of the
heart
• The heart muscle is injured due to not receiving enough
oxygen
Angina
Pectoris
• Chest pain often due to ischemia of the heart muscle
• Due to obstruction or spasm of the coronary arteries
• Main cause improper contractility of the heart muscles
Congestive
Heart Failure
• Congestive cardiac failure or chronic heart failure
• Unable to pump sufficiently to maintain blood flow to meet
the needs of the body
• Most common: Shortness of breath, excessive tiredness
& leg swelling
Summary
• Cardiovascular system consists of the blood, the heart,
and blood vessels
• Heart –
Relatively small, conical organ, located in the mediastinum
• Heart ensures the unidirectional flow of blood through the
blood vessels
• Backflow of blood is prevented by valves within the heart
• Blood that enters an atrium is passed to the ventricle on
the same side of the heart
• Heart chambers and relaxation – Undergo alternate periods
of contraction
• Fossa ovalis:
Oval depression (remnant of the foramen ovale)
• Chordae tendineae:
Tendon like cords- connected to cone shaped trabeculae carneae called papillary
muscles
• As each chamber of the heart contracts – Pushes a volume
of blood into a ventricle or into an artery
• Valves open and close in response to pressure changes as
the heart contracts and relaxes
• The left side of the heart
– Pump for systemic circulation
– Receives bright red, oxygen rich blood from the lungs
• The right side of the heart
– Pump for pulmonary circulation
– Receives all the dark red, deoxygenated blood returning
from systemic circulation
• Components of
conduction system: Sinoatrial (SA) node (pacemaker), Atrioventricular (AV)
node, Atrioventricular (AV) bundle (bundle of His), Bundle branches, Purkinje
fibers
• Cardiac cycle
phases: Atrial systole, ventricular systole, relaxation
• Systole –
Contraction of a heart chamber
• Diastole –
Relaxation of a heart chamber
• Auscultation- Act
of listening to heart sounds
• Blood vessels:
Arteries, arterioles, capillaries, venules and veins
• Three layers of
blood vessel: Tunica interna, tunica media, and tunica externa
• Sympathetic innervation
– Increases the HR and FOC
• Parasympathetic innervation
– Decreases HR, but tends to have no effect on the FOC, except in special
circumstances
• An
electrocardiogram (ECG or EKG): Recording of electrical signals in the
heart
• Blood pressure:
Hydrostatic pressure exerted by blood on the walls of a blood vessel
• Factors affecting
BP: Vascular resistance, VR & velocity
of blood flow
• Two pump blood from
the lower body back to the heart:
The respiratory pump and the skeletal muscle pump
• Echocardiogram:
Uses ultrasound waves to examine the heart
• Regulation of BP:
Neural, hormonal and autoregulation
• The cardiovascular
(CV) center: Group of neurons in the medulla oblongata which regulates HR,
contractility, and blood vessel diameter
• Baroreceptors –
Monitor blood pressure
• Chemoreceptors –
Monitor blood levels of O2 &CO2 and H+ ions
• Sympathetic impulses: Propagated along cardioaccelerator nerves,
increase HR and FOC
• Parasympathetic
impulses: Propagated along vagus nerves, decrease HR
• Disorders: MI,
AP, CHF, arrythmia, hypertension, hypotension