Urinary system
Objectives
At the end of this
lecture, student will be able to
• Describe the functions of urinary system
• Describe the external and internal gross anatomical
features of the kidneys
• Explain the structure of renal corpuscles and renal
tubules
• Explain the basic functions performed by nephrons and
collecting ducts
• Explain the role of renin angiotensin and aldosterone
system in renal physiology
• Describe the mechanisms involved in the maintenance of
acid-base balance
• Compare the roles of buffers, exhalation of carbon
dioxide, and kidney excretion of H+ in maintaining pH of body fluids
• Define acid base imbalance
• Define renal clearance
• Describe various clearance tests for measuring kidney
function
• List the forces that contribute for the flow of urine
through the urinary system
• Describe the anatomy and histology of urinary bladder
• Define “micturition”
• Describe micturition reflux
• Describe the disorders associated with urinary system
Content
• Anatomical features of the kidneys
• Structure of renal corpuscles and renal tubules
• Functions of Nephrons and collecting ducts
• Renin Angiotensin Aldosterone System
• Maintenance of acid-base balance
• Acid-base imbalance
• Renal clearance
• Clearance tests
• Anatomy and histology of urinary system
• Micturition
• Disorders of urinary system
Urinary
system
• Contributes to homeostasis by altering blood composition,
pH, volume, pressure & osmolarity
• Maintenance of blood osmolarity, excreting wastes and
foreign substances, secreting hormones
• Nephrology –
Scientific study of the anatomy, physiology, and pathology of the kidneys
• Urology – The
branch of medicine that deals with the male and female urinary systems
• The urinary system consists of two kidneys, two ureters,
one urinary bladder, and one urethra
Functions
of Urinary system
• Kidney regulate
blood volume, composition & BP
• Synthesize glucose
• Synthesis of hormones: Erythropoietin & calcitriol
• Excrete wastes by forming urine
• Ureters
transport urine from the kidneys to the urinary bladder
• Urinary bladder
stores urine
• Urethra
discharges urine
Anatomy of
Kidney
• Reddish, kidney-bean-shaped organs
• Retroperitoneal
(posterior to peritoneum of the abdominal cavity)
• Located just above the waist between T12 & L3
• Partially protected by the eleventh and twelfth pairs of
ribs
• Right kidney is slightly lower than the left
External
anatomy of Kidney
• 10–12 cm long, 5–7 cm wide, and 3 cm, mass 135–150 g
• Renal hilum – indentation in center of the concave border
• Three layers of tissue surround each kidney
– Renal capsule (deep layer)
– Adipose capsule
(middle layer)
– Renal fascia (superficial layer)
Renal capsule
• Transparent sheet of dense irregular connective tissue
• Serves as a barrier against trauma & helps maintain
the shape
Adipose capsule
• Mass of fatty tissue surrounding the renal capsule
• Protects the kidney from trauma and holds it firmly in
place
Renal fascia
• Thin layer of dense irregular connective tissue
• Anchors the kidney to surrounding structure & to
abdominal wall
Internal
anatomy of Kidney
• Two distinct regions:
– Renal cortex a
superficial, light red area
– Renal medulla
deep, darker reddish-brown inner region
• Renal medulla consists of several cone-shaped renal
pyramids
• Nephrons are the functional units of the kidneys
• 85% – Cortical Nephrons
• 15% – Juxta medullary nephrons
Frontal
section of Kidney
Nephron
• Each nephron consists of two parts:
– Renal corpuscle filters blood plasma
– Renal tubule filtered fluid passes
• Components of a
renal corpuscle
– Glomerulus (capillary network)
– Glomerular (bowman’s) capsule – double-walled epithelial
cup that surrounds the glomerular capillaries
• Components of a
renal tubule
– Proximal convoluted tubule
– Loop of Henle (nephron loop)
– Distal convoluted tubule
Histology
of Renal Corpuscle
Renal
Physiology
• 3 Basic processes
– Glomerular filtration
– Tubular reabsorption
– Tubular secretion
Glomerular
filtration
• The daily volume of glomerular filtrate – 150 L in females
& 180 L in males
• 99% of the glomerular filtrate returns to the bloodstream
via tubular reabsorption
• Only 1–2 liters – excreted as urine
• Filtration fraction
– Fraction of blood plasma in the afferent arterioles of the kidneys
• Glomerular filtrate
– fluid that enters the capsular space
Filtration Membrane
Net Filtration
Pressure
• Glomerular filtration depends on three main pressures
• One pressure promotes filtration and two pressures oppose
• Glomerular blood
hydrostatic pressure (GBHP)
– Blood pressure in glomerular capillaries 55 mmHg
– Promotes filtration by forcing water and solutes in blood plasma
The Opposing Pressure
• Capsular hydrostatic
pressure (CHP) 15 mmHg
• Pressure exerted against the filtration membrane by fluid
already in the capsular space and renal tubule
• Represents a “back pressure”
• Blood colloid
osmotic pressure (BCOP) 30 mmHg
• Due to the presence of proteins in blood plasma:
– Albumin
– Globulins
– Fibrinogen
Net filtration
pressure (NFP)
• Total pressure that promotes filtration
• Determined as follows:
• Net filtration pressure (NFP) = GBHP – CHP – BCOP
= 55 mmHg – 15 mmHg – 30 mmHg
= 10 mmHg
Glomerular Filtration
Rate
• The amount of filtrate formed in all the renal corpuscles
of both kidneys each minute
• In adults, the GFR averages 125 mL/min in males
• 105 mL/min in females
• Regulation of GFR
– Renal autoregulation
– Neural regulation
– Hormonal regulation
Tubular
reabsorption and tubular secretion
Tubular reabsorption:
• Selective process that reclaims materials from tubular
fluid
• Returns them to the bloodstream
• Reabsorbed substances – water, glucose, amino acids, urea,
and ions, such as sodium, chloride, potassium, bicarbonate, and phosphate
Tubular secretion:
• Removed from the blood and discharged into the urine
• Ions (K, H, and NH4), urea, creatinine & certain drugs
Hormonal Regulation
of Tubular Reabsorption and Tubular secretion
Renin–Angiotensin–Aldosterone
System
• Low blood volume and blood pressure
• Juxta glomerular cells secrete the enzyme renin into the
blood
• Sympathetic stimulation releases renin
• Angiotensin converting enzyme (ACE) converts angiotensin I
to angiotensin II (active form)
Effect of
Angiotensin II on renal physiology
• Decreases the glomerular filtration rate
• Enhances reabsorption of Na+, Cl-, and water in the PCT by
stimulating the activity of Na+/H+ antiporters
• Stimulates the adrenal cortex to release aldosterone
• Reabsorb more Na+ and Cl- and secrete more K+ by
stimulating principal cells
• Reabsorbtion of more Na+ and Cl- ; excreting less water;
increases blood volume
Acid-base
balance
• Several mechanisms help maintain the pH of systemic
arterial blood between 7.35 and 7.45
• Homeostasis of H+ concentration within a narrow range is
essential to survival
Removal of H+ from body fluids and its subsequent
elimination depends on
I. Buffer systems
II. Exhalation of
carbon dioxide
III. Kidney excretion of H+
I. Buffer
systems
• Buffers act quickly to temporarily bind H+, remove the
highly reactive, excess H+ from solution
• Buffers raise pH of body fluids but do not remove H+ from
the body
Principal buffer systems are
a. Protein Buffer
System
b. Carbonic
Acid–Bicarbonate Buffer System
c. Phosphate Buffer
System
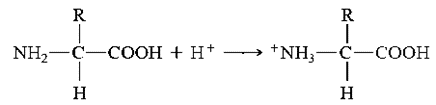
a. Protein
Buffer System
• Buffer in intracellular fluid and blood plasma
• Protein hemoglobin, buffer within red blood cells
• Albumin is the main protein buffer in blood plasma
• Proteins are composed of amino acids
• Contain at least one carboxyl group (COOH) and at least
one amino group (NH2)
• When pH is high – Free carboxyl group at one end of a
protein acts like an acid and releases H+
• When pH is low – Free amino group at the other end of a
protein can act as a base by combining with H+
Hemoglobin as buffer
in red blood cells
• Carbon dioxide (CO2) passes from tissue cells into red
blood cells
• Combines with water (H2O) to form carbonic acid (H2CO3)
• Oxyhemoglobin (Hb
O2) is giving up its oxygen to tissue cells
• Reduced Hb (deoxyhemoglobin) picks up most of the H+
b. Carbonic
Acid–Bicarbonate Buffer System
• The bicarbonate ion (HCO3), act as a weak base
• Carbonic acid (H2CO3), act as a weak acid
When excess of H+ – HCO3
– can function as a weak base and remove the excess H+
When shortage of H+ –
H2CO3 can function as a weak acid and provide H+
c. Phosphate
Buffer System
Components – Ions Dihydrogen phosphate (H2PO4-) and
Monohydrogen phosphate (HPO42-) when pH is high
• Dihydrogen phosphate ion acts as a weak acid and buffer
strong bases such as OH-
When pH is low
• Monohydrogen phosphate ion buffers the H+ released by a
strong acid & acts as a weak base
II.
Exhalation of carbon dioxide
• Increase in the carbon dioxide (CO2) concentration in body
fluids increases H+ concentration and thus lowers the pH
• H2CO3 can be eliminated by exhaling CO2, it is called a
volatile acid
• A decrease in the CO2 concentration of body fluids raises
the pH
III. Kidney
excretion of H+
• In PCT, Na+/H+ antiporters secrete H+ as they reabsorb Na+
• In PCT, Na+/H+ antiporters secrete H+ as they reabsorb
• In collecting ducts, intercalated cells absorb K+ & HCO3; secrete H+
Acid–Base
Imbalances
Normal pH range of systemic arterial blood is between 7.35 –
7.45
Acidosis (or
acidemia)
• Condition where blood pH is below 7.35
• Results in depression of the CNS
Alkalosis
• Conditions where blood pH is above 7.45
• Results in over excitability of the CNS
Clearance
tests
• Measures GFR; useful in assessing renal function
• Volume of plasma that would be completely cleared of a
substance per min
• Clearance (C), expressed as ml/min, can be calculated by
using the formula
C = U х V / P
Where, U = Concentration of substance in urine
V = Volume of urine in ml excreted per min
P = Concentration of substance in plasma
• Measurement of clearance of substance already present in
the blood is preferred
• The compounds measured are: Creatinine and urea
Creatinine clearance
test
• Creatinine is the excretory product derived from
creatinine phosphate
• Its excretion is constant and not influenced by body
metabolism and dietary factor
• It is the volume of plasma that would be completely
cleared of creatinine per min
C =U х V / P
Where, U = Concentration of creatinine in urine
V = Volume of urine in ml excreted per min
P = Concentration of creatinine in plasma
Importance
• Values are close to GFR, hence measurement is sensitive to
assess the renal glomerular filtration
• Decrease in clearance value serves as an indicator of
decreased GFR due to renal damage
Urea clearance test
• Urea is the end product of protein metabolism
• It is the volume (ml) of plasma that would be completely
cleared of urea per min
Cm = U х V / P
Where, Cm = Maximum urea clearence (only when urine output
is > 2 ml/ min
U = Concentration of urea in urine, V = Volume of urine in
ml excreted per min
P = Concentration of urea in plasma
• When urine output is less than 2 ml/min, it is called
standard urea clearence
Cs = U х (V) 1/2
P
• Urea clearence is less than GFR
• After being filtered by glomeruli, it is partially
reabsorbed by the renal tubule
• Influenced by protein content of diet
Importance
• Value below 75%, indicator of renal damage
• If clearance is below 50%, blood urea levels increases
Urine
transportation, storage and elimination
• Urine from collecting duct transported through minor
calyx, major calyx, renal pelvis and later drained into urinary bladder through
ureters
• Urine is then discharged from the body through the single
urethra
Ureters
• Two in number, Retroperitoneal
• 25-30 cm in length; Diameter varies from 1mm to 10mm
• Curved medially & pass obliquely through posterior
aspect of urinary bladder
• Carry urine from renal pelvis to urinary bladder
• Peristaltic contraction, hydrostatic pressure &
gravity are the contributing force for urine flow
Layers of
ureter
3 layers of tissue that form the wall of ureter
– Mucosa; Musclaris; Aventitia
Mucosa
• Mucous membrane with transitional epithelium
• Able to stretch; accommodate variable amount of urine
• Goblet cells produce mucus, prevents cells from coming in
contact with urine
Musclaris
• Intermediate coat
• Has inner longitudinal; outer circular smooth muscle
fibres
• In the distal third, ureter is made of inner longitudinal,
middle circular, outer longitudinal
• Function – Peristalsis
Adventitia
• Superficial coat
• Aerolar connective tissue containing blood vessels,
lymphatic vessels & nerves
• Blends in with the surrounding tissue
• Anchors ureter in place
Urinary
Bladder
• Hollow, muscular organ
• Situated in the pelvic cavity, posterior to pubic
symphysis
• Peritoneum holds the urinary bladder in place
• Usually pear shaped
• Capacity averages 700 – 800 ml
Anatomy and
histology of urinary bladder
• In the floor of urinary bladder is a small triangular
area, trigone
• Two posterior corners of trigone contain two urethral
opening & one external urethral opening, the internal urethral orifice
Layers of
urinary bladder
Walls of urinary bladder, made up of 3 coats
Mucosa
• Mucus membrane with transitional epithelium
• Rugae, permits expansion of urinary bladder
Muscularis/ Detrusor
muscle
• Has 3 layers of smooth muscle fibres – Inner longitudinal;
Middle circular; Outer longitudinal
• External urethral sphincter is made of skeletal muscle
Adventitia
• Layer of aerolar connective tissue
• Continuous with that of uterus
• Over the superior surface of urinary bladder is serosa, a
layer of visceral peritoneum
Micturition
Reflex
• Discharge of urine from urinary bladder is micturition or
urination or Voiding
Volume of urine in
urinary bladder exceeds 200- 400 ml
â
Pressure in bladder
increases
â
Stretch receptors
transmit nerve impulses to spinal cord
â
Impulses reaches
micturition centre in S2, S3
â
Trigger spinal reflex,
Micturition reflex
• Micturition reflex discharge urine from urinary bladder
via parasympathetic impulses
• Contraction of detrusor muscle occur
• Relaxation of internal urethral sphincter muscle
Urethra
• Small tube leading from internal urethral orifice of
urinary bladder to exterior of the body
• Helps to discharge urine from the body
• Anatomy and histology of urethra differ in females and
males
In female,
• Urethra lie posterior to pubic symphysis
• External urethral orifice located between clitoris and
vagina
• Wall consists of deep mucosa and muscularis
In males,
• Urethra extends from internal urethral orifice to the
exterior
• First passes through prostate, then through perineum &
finally through penis
• Wall of male urethra consists of deep mucosa and
superfacial muscularis subdivide into
a. Prostatic urethra – passes through
prostate
b. Membranous urethra – passes through
perineum
c. Spongy urethra – longest portion, passes
through penis
Diseases of
the urinary system
Renal
calculi
• Crystals of salts present in urine occasionally
precipitate and solidify into insoluble stones
• Contains crystals of calcium oxalate, uric acid &
calcium phosphate
Causes –
Ingestion of excessive calcium
– Low water intake
– Abnormally alkaline or acidic urine
– Over activity of parathyroid glands
Urinary
tract infection
• Describes either an infection of a part of urinary system
or presence of large number of microbes in urine
• More common in female due to shorter length of urethra
• Includes urethritis, cystitis, pyelonephritis
Symptoms –
Painful or burning urination
– Frequent
urination
– Low back pain
– Bed wetting
Glomerular
diseases
Glomerulo nephritis
• Inflammation of kidney involving glomeruli
• Due to allergic reaction to the toxins produced by
streptococcal bacteria
• Symptoms – Haematuria, proteinuria
Nephrotic syndromes
• Condition characterised by proteinuria, hyperlipidemia
• Causes- DM, SLE, Cancer & AIDS
• Symptoms- Edema around eyes, ankle, feet and abdomen
Renal
failure
Decrease or cessation of glomerular filteration
Acute renal failure
• Kidneys abruptly
stops working entirely
• Causes – Low blood volume, decreased cardiac output,
damaged renal tubules, kidney stones, NSAIDS
• Symptoms – Oliguria, Anuria, Anaemia
Chronic renal failure
• Progressive and usually irreversible decline in GFR
• Causes – chronic glomerulonephritis, pyelonephritis,
Polycystic kidney disorders, Traumatic loss of kidney tissues
Polycystic
kidney disease (PKD)
• Inherited disorder, kidneys get riddled with 100 – 1000 of
cysts (fluid filled cavities)
• Progressive impairment of renal function leading to end
stage renal failure
Summary
• The organs of the urinary system are the kidneys, ureters,
urinary bladder, and urethra
• Kidneys filter blood and return most water and many
solutes to the bloodstream, the remaining water and solutes constitute urine
• Kidneys are retroperitoneal organs; three layers of kidney
– renal capsule, adipose capsule, and renal fascia
• Nephron is the functional unit of the kidneys
• Nephron consists of a renal corpuscle and a renal tubule
• Nephrons perform three basic tasks: glomerular filtration,
tubular secretion, and tubular reabsorption
• Renal autoregulation, neural regulation, and hormonal
regulation determines the renal function
• Renin angiotensin and aldosterone system helps in
maintaining the blood volume by releasing renin, activating angiotensin II, and
releasing aldosterone
• Various mechanisms help maintain the pH of systemic
arterial blood between 7.35 and 7.45
• Buffers act to temporarily bind H+, removing the highly
reactive, excess H+ from solution
• Increase in concentration of CO2 lowers the pH and will be
reduced by exhalation of CO2
• Kidney excretes excess of H+ ions to maintain the pH of
blood
• Acid- base imbalance causes acidosis and alkalosis
• Various clearance tests helps in measuring the GFR and are
useful in assessing renal function
• Ureters are retroperitoneal and consist of a mucosa,
muscularis, and adventitia
• They transport urine from the renal pelvis to the urinary
bladder, primarily via peristalsis
• Urinary bladder is located in the pelvic cavity; its
function is to store urine before micturition
• Urethra is a tube leading from the floor of the urinary
bladder to the exterior
• Discharge of urine from urinary bladder is micturition
• Micturition reflex discharges urine from the urinary
bladder via parasympathetic impulses
• Diseases associated with urinary system include renal
calculi, urinary tract infection, glomerular disease, renal failure and
polycystic kidney disease