Antihistamines
Intended Learning Outcomes
At the end of the
lecture, students will be able to
• Pharmacology, Chemistry, Biosynthesis of Histamine
• Categorize the antihistamines according to their chemical
structure
• Outline the synthesis of some antihistamines
• Differentiate between 1st generation and 2nd
generation H1 receptor antagonist
• Recognize the specific uses of the different
antihistamines
Histamine
Histamine
–Pharmacology
• Histamine is an Autacoid, which are biological chemicals
which act like local hormones, have a brief duration, and act near their site
of synthesis.
• Histamines has various function in body such as:
– Mediator of inflamation and local immune responses
– regulating physiological function in the gut and
– acting as a neurotransmitter.
• During inflammation Histamine is produced by basophils and
by mast cells, found in nearby connective tissues, which increases the
permeability of the capillaries to white blood cells and some proteins, to
allow them to engage pathogens in the infected tissues
• In the gut it is produced by parietal cells and then
promotes gastric acid secretion and thus aids in digestion. Here it acts like a
local hormone
• As a neurotranmitter, it effects sleeping and waking, food
intake, thermal regulation, emotions and aggressive behavior, locomotion,
memory, and learning
Histamine –
Chemistry
• Histamine is a Nitrogenous base. It is composed of an
imidazole ring and ethylamine side chain. In Plasma pH of 7.4 is exists in
exclusively monocationic form (96.6%). At lower pH higher levels of dication
form exist.
• In solution form, 80% contain H in Nτ tautamer and 20% in
Nπ tautamer
• But crystal form consist primarily of Nτ form
Histamine
Biosynthesis
Note- There some
drugs that can block Histidine Decarboxylase such as Floromethylhistine which
in theory can act as direct acting antihistamine but clinically were found to
be not useful.
Storage and
release of Histamine
• Stored in mast cells in Complex with Heparin
(anticoagulant)
• Stored in basophiles in Complex with Chondrotin
• Histamine as stored in mast cells are found almost
everywhere: skin and the mucosal cells of the bronchi, intestine, urinary
tract, and tissues adjacent to the circulation and within neurons of CNS
• It is released in response to a wide variety of immune
(antigen and antibody) and nonimmune (bacterial products, xenobiotics, physical
effects, and cholinergic effects) stimuli
Histamine
receptors Location and function
H1, H2, H3, H4; they all are GPCR’s
• H1 Location:
CNS neurons, the smooth muscle of respiratory, GIT, uterine tissues, epithelial
and endothelial cells, immune cells
Function:
vasodilation, vascular permeability, hypotension, flushing, pain, headache,
tachycardia, nasal congestion, bronco-constriction, stimulation of cough
receptors, allergic immune response
• Therapeutic usage:
H1 antihistamine are antiallergic, and anti-emetic drugs,
• H1 receptor is 40% similar to muscarinic receptors (thus
some H1 antagonist shows unwanted antimuscaric side effect)
• H1 receptors belong to the superfamily of G protein
coupled receptors (GPCRs), and are encoded for by chromosome 3
• These receptors exhibit spontaneous activation of their
intracellular messengers, requiring no binding by an agonist at surface level
• It exists as a balance between activated (characterized by
the production of intracellular second messengers) and inactive (no such
intracellular signaling) state.
• If the ligand stabilizes the active receptor conformation,
making it the predominant form, then the drug is referred to as an agonist,
while if the inactive conformation is stabilized the drug is said to be a
inverse agonist. In this way, histamine is an agonist, while the antihistamines
are presently considered to be inverse agonists instead of antagonists as
previously believed
• H2 function – gastric acid secretion, vascular
permeability, hypotension, flushing, headache, tachycardia, broncho-dilation
and respiratory mucus production
• Therapeutic use – H2 antihistamines are Anti-ulcer drugs
• H3 Location: CNS
• Function: adrenaline release and autoreceptor of Histamine
in CNS
• Therapeutic use – potential application against obesity
• H4 function: differentiation of hematopoietic cells
• Therapeutic use – none yet
Differentiation
• It is a process by which a less specialized cell becomes a
more specialized cell type
• When cells divide into daughter cells, they are the same
exact cells. This is cell division/growth
• But differentiation means when cells “divide”, different
cell types are formed.
• At conception we all were just a single cell but
differentiation causes us to have diverse specialized cells that make up
different organs
Undifferentiated cell, called stem cells differentiates into diverse
functioning cells
Actions of
Histamine by receptors
Adverse
effects of Histamine
• Drowsiness
• Hypertension
• Urinary Retention
• Vertigo
• Tachycardia
• Dry Mouth
• Increased Appetite
Fig: Effects of H1 antihistamines at histamine, adrenergic, cholinergic,
and serotonin-binding receptors. Many second generation antihistamines do not
enter the brain and, therefore, show minimal CNS effects.
H1
antihistamines
• Their main application is as anti-allergic, anti-emetic
and
• The first generation of H1 antihistamines has sedative
effect due to effect on H1 receptor in brain.
• Structurally this effect is linked to their high
lipophilicity induced BBB penetration and also they are poor substrate for
brain’s endothelial Pglycoprotein efflux pumps, thus can’t exist the brain once
they enter.
• They also antagonize cholinergic receptors which causes
dry mouth, dizziness, fatigue and are alpha adrenergic blockers which can cause
cardiotoxicity by prolonging the QT interval
• The second generation are more selective for H and don’t
penetrate brain and thus has no sedation or cardiotoxicity
• MOA: They bind and stabilize the inactive form of H1
receptors onto which Histamine is not capable of binding.
Therapeutic
Uses: H1 blockers
1. Dermatosis
2. Allergic rhinitis
3. Motion sickness & emesis
4. Parkinson’s disease
5. EPS
6. Insomnia
ECG of
heart and prolonged QT interval
• The QT interval denotes time period taken by heart to
empty it’s blood.
• Prolonged QT interval Suggests problem in cardiac muscle’s
repolarization mechanism after each contraction.
• It is a dangerous side effect that can cause ‘Ventricular
Fibrillation’ which will lead to sudden death unless a defibrillator is used to reset heart’s normal rhythm
Classification
of antihistamines
First Generation Antihistamines
1) Propylamines – Chlorpheniramine, Phenindamine
2) Ethanolamines – Diphenhydramine, Clemastine
3) Ethylenediamines – Pyrilamine, Tripelennamine
4) Phenothiazines – Promethazine, Trimeprazine
5) Piperazines – Cyclizine, Meclizine
6) Heptanes – Azatadine, Cyproheptadine
7) Phthalazinone – Azelastine
Second Generation
(Peripherally Selective) Antihistamines
1) Piperazine- Cetirizine/Levocetirizine
2) Piperidines – Fexofenadine, Loratadine /Desloratadine
Note:
Antihistamines have a lot of structural diversity
Structures
of antihistamines
SAR of H1
antihistamines (1st gen only)
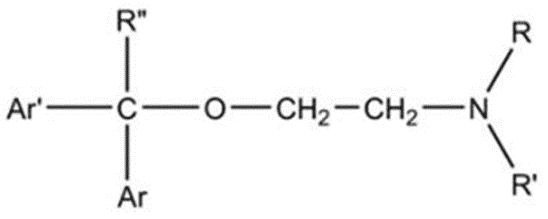
General framework of AntiHistamine (Ethanolamine based)
General framework of Anticholinergics
Note the
similarity in H1 antihistamines and Anticholinergics (this explains the origin
of Anticholinergic side effect of H1 antihistamines)
1. It needs a tertiary amine which is mostly di-methyl
substituted or part of cyclic ring
2. The methylene (-CH2-) groups can be about 2 or 3
3. The oxygen can be removed or replaced with C
4. The terminal carbon must have two aromatic groups and R
group is mostly H but can be CH3 too
5) Alkyl Substitution
in these aromatic rings influence selectivity
• Increasing alkyl substituions at C4 increases anticholinergic
activity and decreases antihistaminic activity
• Increasing alkyl substituions at C2 decreases
anticholinergic activity and modestly increases antihistaminic activity
6) Presence of halogen at C4 position enhances potency
7) Replacement of one of the aromatic rings with
2-pyridyl group increases histaminic selectivity
8) For max potency, the terminal carbon must have R
configuration. R/S configuration at amine is less important
Effect of increasing
Alkyl group at C2 or C4
|
Alkyl |
Anticholinergic |
Antihistaminic |
|
At C2 |
Increases |
Decreases |
|
At C4 |
Decreases |
Increases |
Importance of
stereomeric consideration
|
Configuration |
ED50 |
|
R,R |
0.04 |
|
S,S |
5.0 |
|
R,S |
0.28 |
|
S,R |
11.0 |
Clemastine has two chiral centres, terminal carbon and amine
ED50 reflect potency. Entry 1st and 3rd are most potent.
Both contain R configuration at terminal carbon. Conversely Entry 2nd
and 4th with S configuration at terminal carbon are the least potent
Chlorpheniramine
• It is a propylamine based 1st generation H1
antihistaminic
• It is chlorinated pheniramine which improves potency 10
times and changing toxicity
• It’s Dextro isomer has S configuration and called
DexChlorpheniramine is more potent
• It also acts as serotonin-norepinephrine reuptake
inhibitor or SNRI
• It is combined with opiods for cough medicine because it
can potentiate action of opiods
• It causes drowsiness by penetrating into brain and acting
on H1 receptor
• Uses
– Allergic rhinitis, in cough medicines
Clemastine
• It is an ethanolamine based 1st generation H1
antihistaminic
• This class has a longer duration of action (10-12 hrs)
• It causes drowsiness by penetrating into brain and acting
on H1 receptor
• Uses
– Allergic rhinitis, urticaria (itchy skin rash),
anti-emetic
Pyrilamine
• It is an ethylenediamine based 1st generation
H1 antihistaminic
• They are among the weakest antihistamines
• It is combined with opiods for cough medicine because it
can potentiate action of opiods
• It causes drowsiness by penetrating into brain and acting
on H1 receptor
• Uses
– Allergic rhinitis, incest bites (topically)
Promethazine
• It is a phenothiazine based 1st generation H1
antihistaminic
• It’s sedative action is strong to be used clincally
• It causes drowsiness by penetrating into brain and acting
on H1 receptor
• Uses
– Allergic rhinitis, motion sickness, anti-emetic, sedative
Meclizine
• It is a Piperazine based 1st generation H1
antihistaminic
• It has weak antihistaminic activity
• It causes drowsiness by penetrating into brainand acting
on H1 receptor
• Uses
– Anti-emetic and motion sickness
Cyproheptadine
• It is a Heptane based 1st generation H1
antihistaminic
• It possesses both antihistamine and antiserotonin activity
and is used as an anti-itch agent
• It causes drowsiness by penetrating into brain and acting
on H1 receptor
• Uses
– Allergic rhinitis, allergic conjunctivitis, allergic skin
urticaria, hypersensitivity reactions
Trimeprazine
• Uses
• Antipruritic
– it prevents itching caused by eczema or poison ivy
• It also acts as a sedative,hypnotic
• Antiemetic for prevention of motion sickness
Tripelennamine
Hydrochloride
• First ethylene diamine developed
• Absorbed when given orally
• 2-[benzyl[2-dimethylamino)-ethyl]amino] pyridine
• Allergic rhinitis
• Allergic conjuctivitis
2nd
generation H1 antihistamines
• They don’t act on H1 receptor in brain because their lower
lipophilicity doesn’t allow them to penetrate the BBB
• They have low lipophilicity due to addition of hydrophilic
groups OH, and COOH in the 1st gen molecules. (Other hydrophilic
groups can be NH2,NO2,SO4,PO4)
• They have low affinity for off-targets such as muscarinic,
adrenergic, and serotonergic receptors
• Advantage – negligible sedation, no cardiotoxicity
• Limitation – high selectivity for H1 prevents their use as
anti-emetic, during motion sickness, potentiate cough medicines
Fexofenadine
• It is a piperadine based 2nd gen H1
antihistaminic
• It produces no clinically significant Anticholinergic or
α1-adrenergic blocking or sedative effect at therapeutic doses and is safe even
in higher doses
• It needs only single dosing daily
• Uses
– Allergic rhinitis, chronic urticarial
Cetirizine/Levocetirizine
• It is a Piperazine based 2nd gen H1
antihistaminic
• It produces no clinically significant Anticholinergic or
α1-adrenergic blocking or sedative effect at therapeutic doses
• It needs only single dosing daily
• It’s R-enantiomer, called Levocetrizine, has 30 fold
higher affinity than the S-enantiomer
• Uses
– Allergic rhinitis, relief from urticaria, water eyes
caused by hay fever
Loratidine
Uses
• Hay fever
• To treat cold or allergy symptoms such as sneezing,
itching, watery eyes, or runny nose
• Relieve itching from hives
Summary
• Both the 1st generation drugs and the 2nd
generation drugs are used to treat allergy, hay fever and symptoms of allergy
such as sneezing, itching, watery eyes, or runny nose
• 1st generation drugs have side effects- mainly
it causes drowsiness
• 2nd generation drugs are modified and hence are
mostly devoid of the side effects
• Synthesis of some antihistamines have been outlined