Outpatient Department (OPD)

Outpatient Department (OPD)
Definition of OPD:
OPD is defined as a part of the hospital with allotted physical facilities and medical and other staffs, with regularly scheduled hours, to provide care for patients who are not registered as inpatients.
A hospital department where patients receive diagnosis and/ or treatment but do not stay overnight.
Reasons for Shifting of focus from IP to OP:
– Rising cost of hospital care
– Shortage of hospital beds
– Economic importance
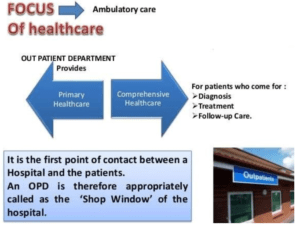
Importance of OPD
- First point of contact.
- It is the shop window of the hospital.
- Makes or mars the image of the hospital.
- A good OPD services can reduce the load on IPD services.
-lt is the place for implementing preventive and primitive health activities.
- It is a stepping stone for health promotion and disease prevention.
- The cost of treatment in 0PD being less than for impatient services
- It is an inseparable link in the hierarchical chain of health care facilities.
- It contributes to reduction in morbidity and mortality.
- Avoidance of the disruption of family life that hospitalization causes.
- Over 30 crore outpatients in a year are treated in the outpatient department of hospitals.
- From 7 to 4 episodes of sickness varying from a mild to moderate to severe nature are suffered by each person in as year.
- Considering that only two episodes out of these may require some kind of medical help, 32 crore episodes (for a population of 16 crore) of sickness would need attending to.
- Only one-sixth to one fifth of these persons manage to seek medical care in the outpatient departments of health centres and hospitals.
- About 25 inpatients are given service per bed in a year.
- On the other hand, for each hospital bed, about 500 outpatients per year are given service.
Objective of OPD
- Modern Techniques for investigation and treatment
- Facilities for total patient satisfaction
- Provide Quality of care
- Good Public relation
- A well-designed and well-organized outpatient department can be high revenue generating area of the hospital.
History of OPD
- Originated in mid-17th century by Sir George Clark.
- in Hotel Dieu in Paris 6 physician ware detailed for regular session on Wednesday or Saturday advising poor individually, in turn introducing the idea of OPD.
- Modern OPD services emerged in 1850 in USA from framework of dispensaries.
Functions of OPD
- An OPD enables a hospital to deliver the following functions:
- Control disease by early diagnosis and timely treatment.
- Investigate and screen cases to confirm whether or not hospitalization is required.
- Facilitate screening and investigations for admission to hospital.
- Provide effective treatment on ambulatory basis.
- Provide follow-up care to discharged patients and their rehabilitation.
- Provide a facility for trainu1g of medical, para-medical and nursing staff.
- It may also provide avenue for epidemiological and social research.
- Control and surveillance of communicable diseases to prevent all outbreak of epidemic.
Preventive Health Activities
- Well baby clinics
- ANC,
- Marriage counselling,
- Family Planning
- School health clinic.
- Control of communicable diseases
- Early diagnosis & detection of chronic diseases like Cancer, TB, and RHD etc.
- Health education & nutritional advice
- Rehabilitation & prevention of disabilities & handicaps
Roles and Functions of OPD
- Specialists Consultation
- Modern Inves. Facility & Treatment
- Refferal for Admission
- Medical Statistics
- Follow Up Care and Rehabilitation
- Training of Med. Students
- Preventive & Promotive Services
- Health Education
Types of OPD
- Two type of OP Services
- Centralized Outpatient Services: All services are provided in a compact area which include all diagnostic and therapeutic facilities being provided in the same place.
- Decentralized Outpatient Services: Services are provided in the respective department.
- Based on type of patient
- General Out Patients: All the patients other than emergencies who report directly to the OPD.
- Emergency Out Patients: A person given emergency medical care for condition which is real or perceived emergency.
- Referred Out Patients: A person referred to an OPD by his attending medical/dental practitioner for specific diagnostic/treatment procedure.
Type of OPD Services
- Ambulatory care is medical care provided on an outpatient basis, including diagnosis, observation, consultation, treatment, intervention, and rehabilitation services. This care can include advanced medical technology and procedures.
- A polyclinic is a clinic that provides both general and specialist examinations and treatments to outpatients and is usually independent of a hospital.
- A health centre is one of a clinics staffed by a group of general practitioners and nurses providing healthcare services to people in a certain area. Typical services covered are family practice and dental care. A walk-in clinic accept patients on a walk-in basis and with no appointment required.
- A day hospital is an outpatient hospital facility where patients attend for assessment, treatment or rehabilitation during the day and then return home or spend the night at a different facility.
- A dispensary is an office in a school, hospital, industrial plant, or other organization that dispenses medications, medical supplies, and in some cases even medical and dental treatment. In a traditional dispensary set- up, a pharmacist dispenses medication as per prescription or order form.
Facilities of OPD
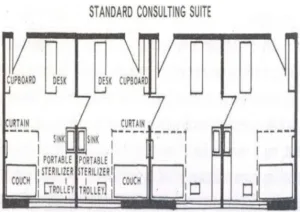
- The Examination Room should be close to the nurse’s station and the consultation room.
- Consultation Room is mostly used when lengthy conversations involved between the doctor and the patient
- The OPD has facilities for screening, counseling, clinical examination, treatment and referral.
It consists of the following:
- Clinical Department of OPD includes clinics which can use standard accommodation, general medicine, surgery, etc
- Types of clinics: surgical, orthopaedic, medical, paediatric skin ophthalmic, ENT dental chest psychiatric, cardiology clinic
- OPD for the surgical department should be located on the ground floor and near the emergency with direct access to it.
- Minor Surgery Room mot be used as a cast room, ECG room, minor operations, should have a separate entrance.
- Support services includes clinics which can use standard accommodation, general medicine, surgery, etc
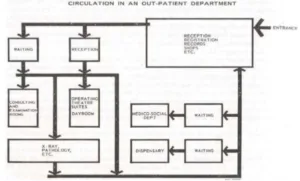
OPD Process
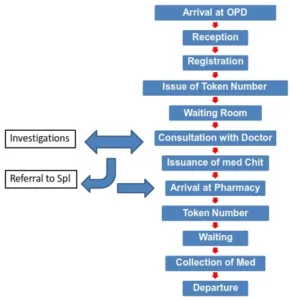
Sources of Origin of Outpatients
- Unreferred Cases
- Discharged Cases from Hospital (follow-up)
- Emergency and Accidents
- Referred Cases from Private Practitioners dispensaries and peripheral hospitals
OPD Planning
- OPD has functional and administrative links with the hospital of which it is a part.
- It may also be linked with Health Centers, Satellite Clinics and Dispensaries dependent on it.
- Expected demand should be determined basing on catchment area and population to be served. Preventive and promotive health
Planning Considerations
After the expected demand has been determined, the following considerations should be taken into account.
- Range of outpatient services to be provided and defining the functions of the outpatient department.
- Daily and hourly capacity required.
- Number of the staff required by category and the tasks required of staff.
- Possible service time per patient, both average and its distribution over various aspects of outpatient
- Flow of patients and work care.
- Requirement of furniture and equipment
- Layout of the department considering all the above.
Key Planning and Design Parameters
- The following are the designing consideration:
- An OPD should be readily accessible from the hospital’s main entrance and people should not have to pass through the wards.
- OPD should be designed either as a centralized polyclinic or decentralized specialty clinic.
- Maybe planned as general OPD or specialty OPD.
- Patients have different degrees of physical and mental abilities.
Patient accessibility should accordingly be designed.
- Effective, comprehensible, and standard signage should be planned.
- Peak hours should be estimated to cater effectively to peak load.
- To make it convenient for patients, the hospital staff and the community, an OPD should be a separate complex within a hospital.
- The location should be such that an OPD shares diagnostic services, such as medical imaging, laboratory, pharmacy, blood bank with other departments of a hospital.
- Toilets should be close to the waiting area. Male and female toilets should be separate.
- A scale of 1-2 WC, for every 100 patients attending OPD and at least one urinal for every 50 patients are recommended.
- Toilets for the staff should also be separate from those for the patients
- Entrance should be near the reception to efficiently answer patient queries.
- Dignity and privacy of patients must be maintained.
- Design should cater for future expansion.
- Educational resource areas for patients education should be integrated in the lobby and waiting areas.
- Design of individual functional areas should extraneous traffic to penetrate any work area. not allow
- Preferably, design should be such that the flow of patients and visitors is unilateral
- Waiting areas and public spaces should be large enough to accommodate patients and accompanying friends and family without causing congestion.
- Sub-waiting areas should be provided adjacent to various clinics.
- Space recommended is 0.8msq per patient for one third of the average daily number of the patients attending OPD in one session.
- Day care facilities may be planned as support services,
- Design should allow natural light and good ventilation.
- It is desirable to provide a good view of the outside
Design Consideration
- Patient accessibility
- Maintain dignity and privacy of patients
- Waiting area and public spaces should be large enough
- Centralized polyclinic or decentralized speciality clinic
- Cater for future expansion
- Day care facilities may be planned as support services
- Effective, comprehensible, standard signage should be planned
- Educational resource areas to be integrated in main lobby
- Should allow natural light and good ventilation.
Requirements for OPD
- 60% of area should be for waiting and corridors.
- Seats for 1/3 of daily attendance @ 8 sq ft/pt.
- Consultation room – 150 sq/ft
- Attached examination room – 80 sq/ft
Projection of Out-Patient Load
- For every hospital bed, 1.5 to 3 patients attend OPD
- 1-10 visits per capita per year of the dependent population basis
Demand for outpatient care varies widely and depends upon
- Cost to the patient,
- Distance,
- Transportation,
- Degree of urbanization,
- Socio-economic status of community,
- Level of facilities and staff, and
- Quality of care provided
Organogram of OPD
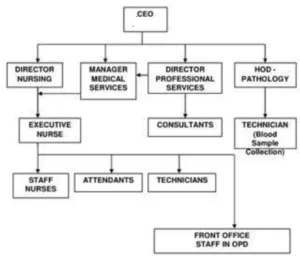
Organizational Components of OPD
Four major organizational components
- Medical staff: Central to the organization
- Nursing staff: Registered nurses, ANMs and nursing or hospital aides
- Ancillary staff: Radiology, laboratory and ECG technicians
- Clerical staff: Carries out registration, billing, receiving cash, secretarial and medical records function.
Planning Consideration
LOCATION-
- Separate entrance
- Easily accessible
- Should have approach from main road
- Adjacent to supportive facilities: x-ray, laboratory
- Amenable for expansion
Organisation of OPD
- Layout and Physical Facility
- Administration Area
- Patient Care
- Public Relation
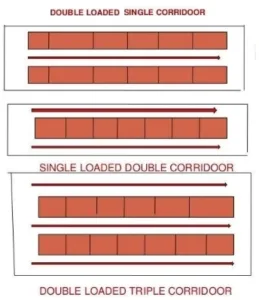
Layout Plan
- Centralized (All services under one roof)
- Decentralized (At different Department)
- Designing (Double loaded single corridor/Single loaded double corridor)
- Location (Near to main gate in & out Gate)
- Size (one Sq ft. per paitent visit/60 sq mt/bed), 2sq mt/bed entrance zone, 10sq mt/bed ambulatory care, 6sq mt/bed Diagnostic zone.
- Entrance Zone – 2 sq.meter/bed.
- Ambulatory zoue-. 10 sq.merer/bed.
- Diagnostic Zone- 6 sq.meter/bed.
- Total hospital area – 60 sq.meter/bed.
PHYSICAL FACILITIES
- Clinical area
- Auxiliary area
- Administrative area
- Ancillary area
- Circulation area
- Public areas
- Physical Facilities
Administrative Areas:
- Admin Office
- Business Office
- House Keeping
- Storage Facility
Circulation Areas (30% of all area):
- Corridors,
- Stairs,
- Lifts
- Easy Accessibility of elevator Corridor- 1.8 m wide
- Security Point
- ATM Card Booth
Hospital Planning and Administration
Ancillary facilities
- Injection room: It should be with waiting area for 10-20 patients with 0.6-0.8 sq. Meter/patient. Area may vary from 12 to 40 sq. Meter depend on work load.
- Treatment & dressing room: About 12-16sq.meter.
- Pharmacy: It should accommodate 5°/o of total clinical visits to OPD in one session
- Health Education Facilities: Min. area required is 15sq.meter.
- Medical Social Service Facilities: should be located in OPD with suitable cubicle for each social worker/Counselor.
- Screening Clinic: required in teaching or tertiary hospital& should be located near reception area having one or more cubicle with 12 sq meter area for each cubicle
Functional Zones
- Public zone
- Main entrance
- Foyer
- Bays for trolleys and wheelchairs
- Public telephone booths
- Public conveniences
- Value added services
- Registration area Cash counter
- Health education facilities
- Joint use zone
- Consultation and examination rooms-combined consultation examination rooms, shared examination room, common pool of shared rooms.
- 12.5 square meter is adequate
Clinical Laboratory
- Centralized sample collection area for urine, stool and blood Wash room, toilets and a blood collection room should be provided.
- In large OPD, routine examination room adjacent to collection station
Pharmacy
- Located so as to serve both inpatients and OPD patients.
Specialised OPD services
- Gastrointestinal endoscopy lab, sigmoidoscopy, colonoscopy.
- Pulmonary function lab
- Cardiac OPD
- Staff Zone
Parking and Entrance
- Main entrance- gentle sloping ramps to facilitate movement
- Entrance should have a double door with a width of 1500mm
- Wheelchairs should be readily available at the entrance
- Staff and patient entrance should be separate Parking should be close to entrance
Enquiry desk, Reception Station
- Height of counter should be adapted to need of wheelchair patients
- To ensure privacy, reception should have counters
Waiting area
- Space recommended is 0.8 square meter per patient for one third of average daily patients attending OPD in one session
- Sub-waiting areas may be shared between the various consultation rooms.
- Distance from waiting area to the consultation room should be short
- Toilets should be Close
PATIENT CARE
- Clinical facilities
- Ambience
- Diagnostic facilities
- Comfort
Standard Consulting Suite
PUBLIC RELATION
- Patient Comfort
- Respect
- Warmth
- Patience Hearing
- Minimum Waiting
- Good Clinical Care
- Cleanliness
- Good Ambience
- Canteen Toilet, Ventilation Water Supply
Specialized OPD
- Specialized OPD services may include the following;
- Gastrointestinal endoscopy lab, sigmoidoscopy and colonoscopy.
- Pulmonary Function Lab including spirometery
- Cardiac OPD with ECG, Echocardiography, TMT and Holter Monitoring Lab. (Treadmill Test)
Problems at OPD
General Problems:
- Insufficient number of doctors: It is found that there are a significant large number of patients wait in front of the doctor rooms. it can be concluded that this is the bottleneck of the process. This is mainly due to insufficient number of doctors to serve as compared to the number of patients arrive the clinic.
- Inappropriate appointment system: Appointment-patient has no priority over non-appointment patient. Two types of patients follow the same process. Therefore, appointment-patients are likely to ignore their appointment time and tend to arrive the clinic very early. This causes congestion in the clinic during the beginning of the day. Moreover, there is no formal appointment system in place. There is no time slot information to guarantee the availability of doctors on the appointment day.
- Long waiting time at Medicine room: After patients receive the prescription from the clinic counter, patients are directed to medicine room to pay for the fee and receive the medicines. According to our observation, patients currently spend significant amount of time at the medicine room counter. Most of which is waiting for medicine.
- Shortage of facilities.
- Insufficient training of medical personnel concerning ambulatory care.
- Fragmentation of care, poor communication and inadequate understanding of their demands.
- An organizational structure geared to traditional preferences and needs of the providers.
- Resistance to change.
Specific Problems:
- Duties undertaken by the auxiliaries are carried out hurriedly in order to keep pace with consultation of doctors. This creates inappropriate documentation.
- Auxiliary staffs sometimes misbehave with the patients.
- In absence of appointment system, patients start accumulating even before office time starts; creating a long queue of patients even before arrival of doctors.
- Absence of visible serial number of appointment.
- Interruption of consultation or investigation.
- Lack of privacy.
- Advices are not clearly spelled out.
- Illegible hand-writing of the doctors.
- Poly-pharmacy.
- Prescription of too much antibiotics.
- Queues are not properly maintained.
- Prescribed medicines are not always available at pharmacy.
- Use of trade-name of medicines by the doctors, create confusion to patients, when different-named medicines of same genera is supplied to the patients.
- No clear advice about when, how and how long to take the medicines.
- Sometimes, wrong medicines are given by the pharmacists.
- Insufficient and un-cleaned toilets.
- Undue influence of local political leaders.
Managerial Considerations
- Policy & Guidelines
- Over Crowding
- Quality of Care
- Proper Management Structure
- Staff Training Motivation
- Monitoring Evaluation
- Direction Sign/ Information Graphic
- Appointment System
- Good Public Relation
How to Deal With Long Waiting Time
Stages where delay occurs:
- Registration Preparation of medical record Collection/payment of fees
➤ annoying to the patients and bad public relations for the Hospital
➤ Large number of patients not the only reason for people waiting.
Over Crowding and Long Waiting
How to Solve Over Crowding?
- Split OPD
- Central Registration System
- Screening Centres
- Queing Theory
- More Consultation Rooms
- More Regn. Counter
- Appointment System
Normal Queue System
- Make queue attractive.
- Make waiting-lines bent, so that they don’t see a long line of queue always ahead of them. Give them hope.
- Keep provision of visible token-number; so that one can predict his turn of appointment.
- People always remember the last part of service.
So provide a satisfying consultation.
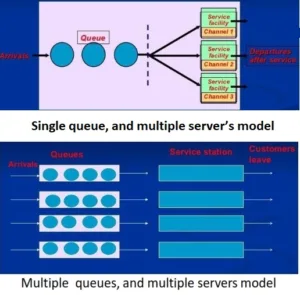
Suggestions for managing queues
- Determine an acceptable waiting time for customer.
- Try divert customer’s attention when waiting.
- Inform customers of what to expect.
- Keep employees not serving the customers out-of-sight.
- Train servers to be friendly.
- Encourage customers to come during slack period.
- Identify the bottle-neck in the service delivery and take remedial measures.
Records at OPD
- Clinical Records supposed to be kept
- OPD registration record
- Treatment record
- Medication Record
- Report of investigations
- Consent forms
(All records are supposed to keep for three years)
Policy and Guidelines
- Sustained and continuity of high standard patient care.
- Modern technology and methods.
- Obtain total patient satisfaction.
- Highly motivated and trained, skilled hospital staff.
- Manual of procedures for hospital staff.
- Periodic training and review system.
- Recording and retrieval system.
- System of appointment
- Morning and afternoon clinics
- Proper Sinage System
Also, Visit:
B. Pharma Notes | B. Pharma Notes | Study material Bachelor of Pharmacy pdf