SULFONAMIDES
The first antimicrobials effective against Pyogenic
Bacterial infections.
Derivatives of Sulfanilamide containing a “sufonamido “ring
(SO2NH2).
Structurally and chemically related to p-aminobenzoic acid (PABA).
Structurally similar to many drugs – thiazides,
acetazolamide, dapsone and sulfonylureas etc.
Physically – available as white powder, mildly acidic and form
water soluble salts with bases.
However, indications and practical uses are very few these
days.
Sulfonamides – Classification
Short acting:
Sulfadiazine, Sulfadimidine, Sulfacetamide
Intermediate acting:
Sulfamethoxazole
Long acting:
Sulfadoxine, Sulfamethoxypyrazine, Sulfadimethoxine etc.
Topically used:
Mafenide, Silver sulfadiazine and Sulfacetamide
Ulcerative colitis:
Sulfasalazine
Sulfonamides – Antibacterial Property
Bacteriostatic against gm +ve and gm –ve bacteria
Bactericidal in urine
Susceptible
organisms: Str. pyogens, H. influenzae, H. ducreyi, Callymatobacterium
grannulomatosis, V. cholerae, Chlamydia, Actinomyces etc.
Few strains of Staph aureus, gonococci, meningococci,
pneumococci, E. coli and Shigella
Chlamydiae:
trachoma, lymphogrnuloma venereum. Inclusion conjunctivitis. Also Actinomyces
and Nocardia
Protozoa:
Plasmodium (Sulfadoxine + Pyrimethamine)
Toxoplasmosis (Sulfadiazine + Pyrimethamine)
PCP (Sulfamethoxazole + Trimethoprim = SXT)
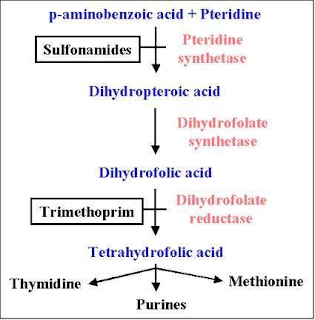
Sulfonamides – MOA
Sulfonamides – Resistance
Many strains – S. aureaus, pneumococci, gonococci,
meningococci, Strep. Pyogens, E. coli and Shigella
Mechanism:
1.
Production of increased amounts of PABA
(Staph, Neisseria)
2.
Folate synthase enzyme has low affinity to
sulfonamides.
3.
Adopt alternative pathway of folate synthesis –
structural changes in folate synthase (E
coli) – encoded chromosomally and
plasmid mediated
Resistant to one sulfonamide – resistant to all
No cross resistance
Sulfonamides – Kinetics
Rapidly and completely absorbed from GIT
Extend of plasma protein binding differs (10 –95%)
Longer acting ones are highly plasma protein bound
Widely distributed – enters in serous cavity easily
Metabolized by non-microsomal acetyl transferase in liver –
slow and fast acetylators
Acetylated product – inactive excreted in urine (but, more
toxic than parent) – crystalluria
Acetylated form accumulates in blood – toxic in renal faiure
Reabsorbed in tubule
Sulfonamides – ADRs
Nausea, vomiting and epigastric pain
Crystalluria – alkanization of urine
Hypersensitivity (2 – 5%) – rashes, urticaria, drug fever.
Exfoliative dermatitis, SJ syndrome (long acting ones)
Hepatitis
Haemolysis – G-6-PD deficiency
Kernicterus – displacement of bilirubin
Individual Sulfonamides
Sulfadiazine:
General purpose use – absorbed orally and rapidly excreted. More crystalluria.
Preferred in meningitis.
Sulfamethoxazole:
slower absorption and lower excretion. 10 Hrs.
Half-life. Combination with Trimethop
Sulfadoxine: Ultra-long
acting >1 week. High protein bound – long excretion. Not suitable for pyogenic
infections – low plasma conc. Used in
Malaria, Pneumocystis jiroveci and toxoplasmosis
Sulfacetamide:
Ophthalmic use – infections by bacteria, chlamydia, ophthalmia neonatorum etc
Mafendie:
Atypical sulfonamide. Local application – inhibits variety of bacteria – active
in presence of pus – pseudomonas and clostridia
Silver sulfadiazine:
Bacteria, fungi, Pseudomonas. In burn cases
Sulfonamides – Uses
Rarely used now a days systemically
UTI: caused by E. coli and P. mirabilis: Sulfisoxazole – 1
gm 4 times daily
Malaria: sulfadoxine and pyrimethamine combination
Toxoplasmosis: sulfadiazine + pyrimethamine
In Combination with Trimethoprim: Cotrimoxazole
Ulcerative colitis: Sulfasalazine – 1-4 gm initially and 500
mg 6 Hrly.
Locally:
Sodium sulfacetamide: 10-30% ophthalmic solution in
bacterialconjunctivitis, trachoma etc.
Mafenide acetate (1% cream) and Silver sulfadiazine 1%
cream): Burn dressing and chronic ulcers
Trimethoprim
Trimethoprim (trimethyl benzyl pyrimidine) is a
diaminopyrimidine, chemically related to Pyrimethamine
Do not confuse: Clotrimazole (antiungal) – Cotrimoxazole is
TMP – SMZ, but Sulfadoxine + Pyrimethamine is antimalarial
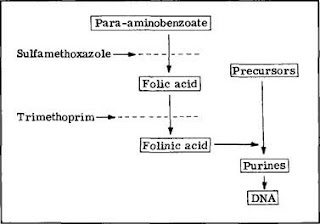
MOA: Sequential block of folate metabolism
Trimethoprim is 50,000 or more times more active against
bacterial DHFRase enzyme than mammalian
So, no harm to human folate metabolism
MOA OF TRIMETHOPRIM-SULFAMETHOXAZOLE
Cotrimoxazole –
general points
Individually, both are bacteriostatic, but combination is –
bactericidal
Both drugs have almost similar half-lives (10 Hrs)
Maximum synergism if the organism is sensitive to both the agents.
Optimal synergism is obtained at 20 (S): 1 (T) concentration
(MIC of both is reduced by 3 – 6 times)
1.
This ratio is obtained at 5:1 dose ratio (e.g.
800 mg: 160 mg)
2.
Because TMP has large Vd and enters many tissues
– plasma conc. is low
But, TMP crosses BBB and placenta and SMZ not
TMP is more rapidly absorbed than SMZ
TMP is 45% plasma protein bound but SMZ is 65% bound
TMP is partly metabolized in liver
Cotrimoxazole –
antibacterial spectrum
Similar to sulfonamides
Additional benefits: Salmonella typhi, Serratia, Klebsiella
Enterobacter, Yersinia and Pneumocystis jiroveci
– Sulfonamides resistance strains of S. aureus, E. coli,
gonococci, meningococci and H influenza
RESISTANCE: Slow to develop
– By mutational changes or plasmid mediated acquisition of a
DHFRase enzyme having lower affinity for the inhibitior.
Cotrimoxazole –
ADRs
All adverse effects of sulfonamides – nausea,
vomiting,stomatitis,rash etc
Folate deficiency (megaloblastic anaemia) – patients with
marginal folate levels
Blood dyscrasias
Pregnancy: teratogenic risk, Neonatal haemolysis and methaemoglobinaemia
Patients with renal disease may develop uremia
Fever, rash and bone marrow hyperplasia
Elderly – risk of bone marrow toxicity from cotrimoxazole
Diuretics given with cotrimoxazole have produced a higher incidence
of thrombocytopenia
Bone marrow hypoplasia among AIDS patients with Pneumocystis
jiroveci infection
Cotrimoxazole –
Uses
Uncomplicated infection of the lower urinary tract infection
– Cystitis (5 tablet dose)
– Chronic and recurrent urinary tract infections (including
enterobacteriaceae) – 3-10 days
Respiratory tract infection – lower and upper, chronic
bronchitis, facio-maxillary infections, otitis media due to gm+ve cocci and H
influenzae etc
Typhoid
Bacterial diarrhoeas & dysentery: due to campylobacter,
E coli, Shigella etc.
Pneumocystis jiroveci: Severe pneumonia – Prophylactic use
in AIDS patients with neutropenia. Dose – DS tablet 4-6 times 2-3 weeks
Chancroid – H. ducreyi
Alternative to penicillin in agrannulocytosis patients, scepticaemia
etc.