Anti-hypertensive Drugs

Etiology of Hypertension
A specific cause of hypertension established in only 10–15% of patients.
Patients in whom no specific cause of hypertension are said to have essential or primary hypertension.
Patients with a specific etiology are said to have secondary hypertension.
Genetic factors, psychological stress, and environmental and dietary factors contribute to the development of hypertension. The heritability of essential hypertension is estimated to be about 30%.
Classification of hypertension based on blood pressure
Normal Regulation of Blood Pressure
Blood pressure is maintained by
Anti-hypertensive Drugs
Anti-hypertensive drugs are medications used to treat high blood pressure, also known as hypertension. These drugs work by various mechanisms to lower blood pressure and reduce the risk of complications associated with hypertension.
Classification of Antihypertensive agents
1. Diuretics
Thiazides: Hydrochlorothiazide, Chlorthalidone, Indapamide
High ceiling: Furosemide, Torsemide, ethacrynic acid.
K+ Sparing: Spironolactone, Amiloride
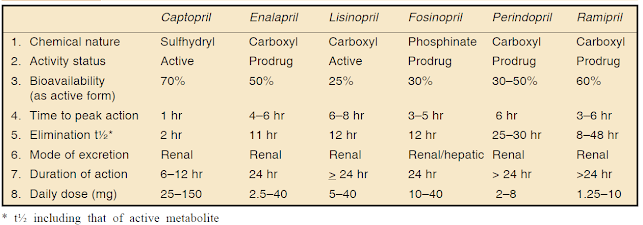
2. ACE inhibitors
Captopril, Enalapril, Lisinopril, Perindopril, Ramipril, Fosinopril, etc.
3. Angiotensin (AT1 receptor) blockers:
Losartan, Candesartan, Irbesartan, Valsartan, Telmisartan
4. Direct renin inhibitor:
Aliskiren
5. β Adrenergic blockers:
Propranolol, Metoprolol, Atenolol, etc.
6. Calcium channel blockers:
Verapamil, Diltiazem, Nifedipine, Felodipine, Amlodipine, Nitrendipine, Lacidipine, etc.
7. β + α Adrenergic blockers:
Labetalol, Carvedilol
8. α Adrenergic blockers:
Prazosin, Terazosin, Doxazosin, Phentolamine, Phenoxybenzamine
9. Central sympatholytics:
Clonidine, Methyldopa
10. Vasodilators
Arteriolar: Hydralazine, Minoxidil, Diazoxide
Arteriolar + venous: Sodium nitroprusside
11. Others:
Adrenergic neuron blockers (Reserpine, Guanethidine, etc.), Ganglion blockers (Pentolinium, etc.)
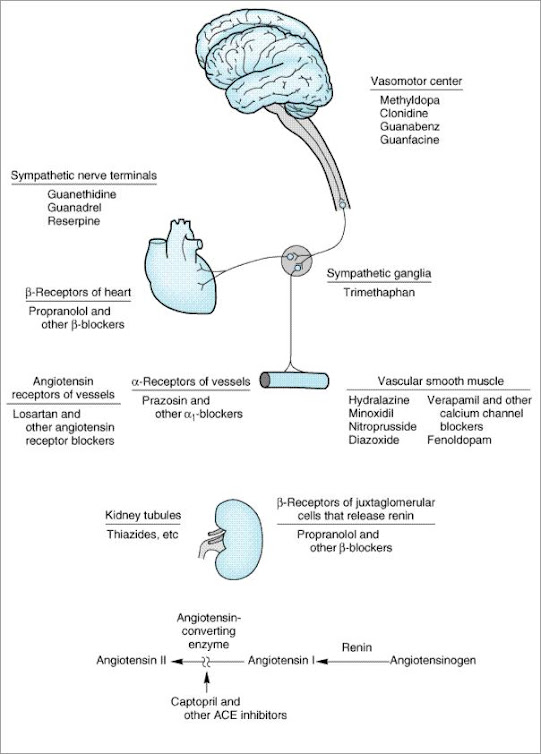
Sites of action of the major classes of anti-hypertensive drugs
Diuretics
Thiazide diuretics:
Loop diuretics:
K+ Sparing:
ACE inhibitors
Advantages of ACE inhibitor:
Uses of ACE inhibitors
1. Hypertension:
The ACE inhibitors are first-line drugs in all grades of hypertension, but the angiotensin receptor blockers (ARBs) have now surpassed them in popularity.
Essential hypertension responds to monotherapy with ACE inhibitors and the majority of the rest to their combination with diuretics or beta blockers.
2. Congestive Heart Failure (CHF):
ACE inhibitors cause both arteriolar and vasodilatation in CHF patients; reduce afterload as well as preload.
3. Myocardial infarction:
Long-term ACE inhibitor therapy reduces recurrent MI.
4. Prophylaxis in high cardiovascular risk subjects:
ACE inhibitors are protective in high cardiovascular-risk subjects even when there is no associated hypertension or left ventricular dysfunction. ACE inhibitors may improve endothelial function.
5. Diabetic nephropathy:
Prolonged ACE inhibitor therapy has been found to prevent or delay end-stage renal disease in type I as well as type II diabetics.
6. Nondiabetic nephropathy:
ACE inhibitors reduce proteinuria by decreasing the pressure gradient across glomerular capillaries and altering membrane permeability.
7. Scleroderma crisis:
The marked rise in BP and deterioration of renal function in the scleroderma crisis is mediated by Ang II.
ACE inhibitors produce improvement and are life-saving in this condition.
Adverse effects of ACE inhibitors:
Angiotensin antagonists (ARBs)
losartan, candesartan, valsartan, telmisartan, olmesartan and irbesartan.
The pharmacologic effects of ARBs are similar to those of ACE inhibitors.
ARBs produce arteriolar and venous dilation and block aldosterone secretion, thus lowering blood pressure and decreasing salt and water retention.
ARBs do not increase bradykinin levels.
ARBs may be used as first-line agents for the treatment of hypertension, especially in patients with a compelling indication of diabetes, heart failure, or chronic kidney disease.
Direct renin inhibitor
β-adrenergic blockers
β-adrenergic blockers are mild antihypertensives and do not significantly lower BP in normotensives.
In stage 1 cases of hypertensive patients (30 – 40%), β- adrenergic blockers are used alone.
Propranolol
Propranolol is the first β blocker shown to be effective in hypertension and ischemic heart disease.
Propranolol has now been largely replaced by cardioselective β blockers such as metoprolol and atenolol.
All β-adrenoceptor-blocking agents are useful for lowering blood pressure in mild to moderate hypertension.
In severe hypertension, β blockers are especially useful in preventing the reflex tachycardia that often results from treatment with direct vasodilators.
Metoprolol & Atenolol
Metoprolol and atenolol, which are cardioselective, are the most widely used β blockers in treating hypertension.
Metoprolol is atenolol inhibiting stimulation of β1 adrenoceptors.
Sustained-release metoprolol is effective in reducing mortality from heart failure and is particularly useful in patients with hypertension and heart failure.
Atenolol is reported to be less effective than metoprolol in preventing the complications of hypertension.
Other beta blockers
α-Adrenergic blockers
Prazosin, terazosin, and doxazosin
Prazosin is a prototype α1-adrenergic blocking agent.
Terazosin and doxazosin are long-acting congeners of Prozosin.
Alpha-blockers reduce arterial pressure by dilating both resistance and capacitance vessels.
Other alpha-adrenoceptor blocking agents
phentolamine (reversible nonselective α-adrenergic antagonist) and phenoxybenzamine (a non-selective, irreversible alpha-blocker) are useful in the diagnosis and treatment of pheochromocytoma.
Centrally-acting adrenergic drugs
Clonidine
Clonidine acts centrally as an α2 agonist to produce inhibition of sympathetic vasomotor centers, decreasing sympathetic outflow to the periphery.
This leads to reduced total peripheral resistance and decreased blood pressure.
At present, it is occasionally used in combination with a diuretic.
Methyldopa
Vasodilators
Treatment of hypertension
FAQs
- How quickly do anti-hypertensive drugs work? Anti-hypertensive drugs may start showing effects within a few hours to days, but the full impact may take weeks.
- Can lifestyle changes alone manage hypertension? While lifestyle changes are crucial, some individuals may require medication for optimal blood pressure control.
- Are there natural alternatives to anti-hypertensive drugs? While lifestyle modifications can complement treatment, they may not replace the need for medication in severe cases.
- What should I do if I experience side effects from my medication? Consult your healthcare provider immediately; they can adjust your medication or suggest alternative options.
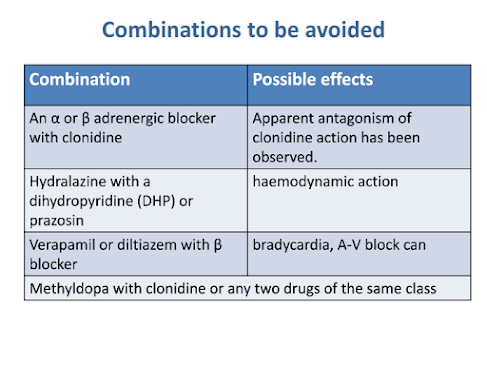
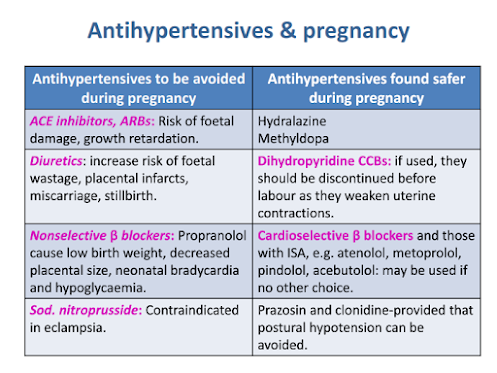
- Is it safe to combine different types of anti-hypertensive drugs? Combining drugs can be safe and effective, but it should be done under the guidance of a healthcare professional.
Anti-hypertensive Drugs Notes PDF
Also, Visit:
B. Pharma Notes | B. Pharma Notes | Study material Bachelor of Pharmacy pdf