Lymphatic system
Objectives
At the end of this
lecture, student will be able to
• List the components of the lymphatic system
• Explain major functions of the lymphatic system
• Describe the organization of lymphatic vessels
• Explain the formation and flow of lymph
• Differentiate the primary and secondary lymphatic organs
and tissues
• Explain the anatomy of thymus and lymph node
• Describe the anatomy of spleen
• List the lymphatic nodules
• Discuss the disorders of Lymphatic system
Content
• Components of lymphatic
system
• Lymphatic ducts and trunks
• Formation and flow of lymph
• Primary and secondry lymphatic organs
• Spleen
• Lymphatic nodule
• Disorders
Lymphatic
System
• Consists of
– A fluid called lymph
– Vessels – lymphatic vessels
• Lymphatic tissue
– Specialized form of reticular connective tissue
– Contains large numbers of lymphocytes
– B cells and T cells (Adaptive immunity)
Blood
Plasma to Lymph
Difference between interstitial fluid and lymph is location
Functions
of Lymphatic System
• Removal of excess
fluids
– Lymphatic vessels drain excess interstitial fluid from
tissue spaces
• Transports dietary lipids
– Transport lipids and lipid-soluble vitamins (A, D, E, and
K) absorbed by GIT
• Carries out immune responses
– Initiates high specified responses
– Directed against particular microbes or abnormal cells
Lymphatic vessels
• Lymphatic
Capillaries
– Located in the spaces between cells
– Closed at one end
– Unite to form larger lymphatic vessels
– Resemble veins in structure
– Thinner walls and more valves
• At intervals, lymph flows through lymph nodes
Tissues
that lack lymphatic capillaries
• Include avascular tissues:
– Cartilage
– Epidermis
– Cornea of the eye
• CNS
• Portions of the spleen
• Portions of Red bone marrow
Details of
a Lymphatic Capillary
Lacteals
• In small intestine, specialized lymphatic capillaries –
lacteals
• Carry dietary lipids into lymphatic vessels and ultimately
into the blood
• Presence of lipids causes the lymph draining from the
small intestine to appear creamy white – Chyle
• Elsewhere, lymph is a clear, pale-yellow fluid
Details of
Lymphatic Capillary
Lymph
Trunks and Ducts
Lymph passes from lymphatic capillaries into lymphatic vessels,
then through lymph nodes in a particular region of the body
Unite to form lymph trunks
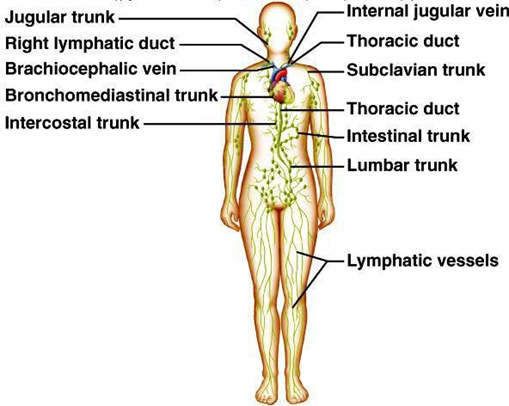
The
Principal Trunks
• Lumbar
• Intestinal
• bronchomediastinal
• Subclavian
• Jugular trunks
Lymph
Trunks
• The lumbar trunks
– Drain lymph from the lower limbs, viscera of the pelvis
– Kidneys, adrenal gland abdominal wall
• The intestinal trunk
– drains lymph from the stomach, intestines
– Pancreas, spleen, and part of the liver
• The bronchomediastinal
– Trunks drain lymph from the thoracic wall, Lung, heart
• The subclavian trunks – Drain the upper limbs
• The jugular trunks – Drain the head and neck
Lymph Ducts
• Lymph passes from lymph trunks into two main channels:
– The thoracic duct
– The right lymphatic duct
The Right Lymphatic
Duct
• Receives lymph from the upper right side of the body
The Thoracic Duct
• Main duct for the return of lymph to blood
Thoracic
Duct
• Begins as a dilation called the cisterna chyli
• Receives lymph from the left side of the head, neck, and
chest, the left upper limb, and the entire body inferior to the ribs
• Drains lymph into venous blood at the junction of the left
internal jugular and left subclavian veins
The Right
Lymphatic Duct
• Receives
– Lymph from the upper right side of the body
• Drains
– Into venous blood at the junction of the right internal
jugular and right subclavian veins
Formation
and Flow of Lymph
Blood plasma filter freely through the capillary walls
From interstitial fluid- small amount of proteins
(reabsorbed)
Excess filtered fluid— about 3 l/day—drains into lymphatic
vessels – Lymph
Proteins that do leave blood plasma cannot return to the
blood by diffusion
Thus, important function of lymphatic vessels is to return
the lost plasma proteins to the bloodstream
The
sequence of fluid flow
Blood capillaries
Interstitial spaces
Lymphatic capillaries
Lymphatic vessels
Lymphatic ducts
Junction of the internal jugular and subclavian veins
(blood)
Flow of
Lymph – Skeletel Muscle Pump
• The milking action compresses lymphatic vessels (as well
as veins)
• Forces lymph toward the junction of the internal jugular
and subclavian veins
Flow of
Lymph- Respiratory Pump
• During inhalation – Lymph flows from the abdominal region
to thoracic region
• During exhalation – The valves
Lymphatic
Organs and Tissues
Primary lymphatic
organs
• Stem cells divide and become immuno competent – capable of
mounting an immune response
• Organs
– Red bone marrow
– Thymus
The secondary
lymphatic organs and tissues
• The sites where most immune responses occur
• Lymph nodes
• Spleen
• Lymphatic nodules (follicles)
Red Bone
Marrow
• Pluripotent stem cells in red bone marrow give rise to mature:
• immuno competent B cells
• Pre-T cells
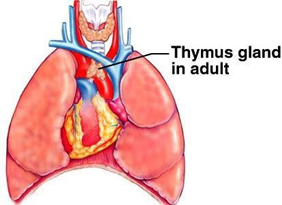
Thymus
Anatomy
• Bilobed organ located in the mediastinum
An enveloping layer of connective tissue holds the two lobes
closely together
• Trabeculae
Extensions of the capsule
– Penetrate inward and divide each lobe into lobules
Each thymic lobule
consists of:
• The cortex
– Large numbers of T cells
• The medulla
– Widely scattered, more mature T cells, epithelial cells,
dendritic cells, and macrophages
Thymus –
Cells
• Dendritic cells
– Assist the maturation process of T cells
• Epithelial cells
– Serve as a frameworks
– Help educate the pre-T cells in positive selection
– Produce thymic hormones – aid in the maturation of T
cells.
• Macrophages
– Help clear out the debris of dead and dying cells
The surviving T cells enter the medulla
Thymic
Hassall’s Corpuscles
• Some of the epithelial cells become arranged into
concentric layers of flat cells
• Serve as sites of T cell death in the medulla
• Degenerate an d become filled with keratohyalin granules
and keratin – Clusters – Thymic Hassall’s Corpuscles
Fate of T
Cells
• T cells that leave the thymus via the blood
• Migrate to:
– Lymph nodes
– Spleen
– Other lymphatic tissues
• Colonize parts of those organs and tissues
Lymph Nodes
• Located along lymphatic vessels – 600 bean-shaped lymph
nodes
• Scattered throughout the body superficial and deep (in
groups)
• Large groups of lymph nodes – Near the mammary glands and
in the axillae and groin
• Small, round or oval structures located along the pathways
of lymph vessels
Lymph Node
– Anatomy
• Lymph nodes are 1–25 mm long
• Covered by a capsule of dense connective tissue
• Stroma
– The capsule,
trabeculae, reticular fibers, and fibroblasts
• Supporting network:
– Internal to the capsule
– Reticular fibers, and fibroblasts
• Trabeculae:
– Divide the node into compartments & provide support
– Provide a route for blood vessels into the interior of a
node
The
Parenchyma (Functioning Part)
Superficial cortex
Deep medulla
Lymph Nodes
Function
• As a type of filter
• Reticular fibers
– Foreign substances are trapped the reticular fibers within the
sinuses of the lymph node
• Macrophages
– Destroy foreign substances by phagocytosis
• Lymphocytes
– Destroy by immune responses
Spleen
• Oval shaped
• Largest single mass of lymphatic tissue in the body
• Located in the left hypochondriacs region
The superior surface
• Smooth and convex
• Conforms to the concave surface of the diaphragm
Visceral surface
• Neighboring organs make indentations
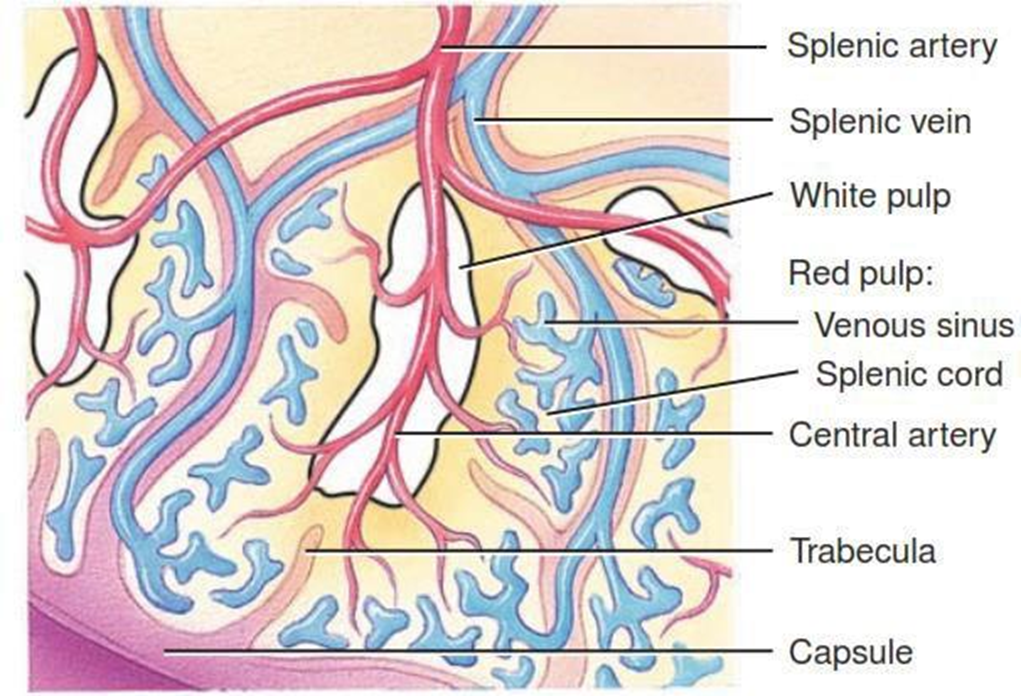
Spleen –
Anatomy
• A capsule – dense connective tissue surrounds the spleen
• Covered by a serous membrane – the visceral peritoneum
• Trabeculae extend inward from the capsule.
• Stroma: The capsule, trabeculae, reticular fibers &
fibroblasts
Internal
Structure of Spleen
Parenchyma:
2 types of tissue white pulp and red pulp
White Pulp
• Lymphatic tissue – consisting mostly of lymphocytes and macrophages
• Arranged around central arteries
• Blood flow – to the splenic artery enters the central
arteries
Red Pulp
• Consists of:
– Blood-filled venous sinuses
– Cords of splenic tissue called splenic (Billroth’s) cords
– Veins are closely associated with the red pulp
• Splenic cords
Consist of:
– Red blood cells
– Macrophages
– Lymphocytes
– Plasma cells
– Granulocytes
Internal Structure of
Spleen
• Within the white pulp
– B cells and T cells carry out immune responses
– Macrophages destroy blood-borne pathogens by phagocytosis
• Within the red pulp
– Macrophages: Removed raptured, worn out, or defective blood
cells and platelets
– Storage of platelets
– Production of blood cells (hemopoiesis) during fetal life
Lymphatic
Nodules
• Egg-shaped masses of lymphatic tissue
• Not surrounded by a capsule.
• Scattered throughout the lamina propria of mucous
membranes lining:
– GIT
– Urinary and reproductive tracts
– Respiratory airways
• MALT – Mucosa-associated lymphatic tissue
• Many lymphatic nodules are small and solitary
• Some lymphatic nodules occur in multiple large
aggregations in specific parts of the body
– Tonsils in the pharyngeal region strategically positioned
to participate in immune responses
– The aggregated lymphatic follicles (Peyer’s patches) in
the ileum
Nonspecific
and Specific Defenses
• Immunity involves nonspecific and specific defenses
Nonspecific defenses
• Include barriers to entry, the inflammatory reaction, NK
cells & protective proteins
Specific defenses
• Requires B lymphocytes and T lymphocytes
• B cells undergo colonal selection with production of
plasma cells
• Memory B cells – Combine with a specific Ag
T cells
• Responsible for cell mediated immunity
• The two main types: Cytotoxic T cells & helper T cells
• Cytotoxic T cells – Kill virus-infected or cancer cells on
contact
• Helper T cells – Produce cytokines and stimulate other
immune cells
Induced Immunity
• Immunity can be induced in various ways
• Vaccines are available to induce long-lasting, active
immunity
• Antibodies – Temporary, passive immunity
Antigen-
Presenting Cell
• For a T cell to recognize an antigen, the antigen must be
presented by an antigen-presenting cell (APC)
• Thereafter, the activated T cell undergoes colonal
expansion
• Then most of the activated T cells undergo apoptosis
• A few cells remain
as memory T cells
Summary
• The lymphatic network begins with microscopic vessels called
lymphatic capillaries
• Lymphatic tissue is specialized form of reticular
connective tissue, contains large numbers of lymphocytes
• Specialized lymphatic capillaries in small intestine are
known as lacteals
• Lymph passes from lymph trunks into two main channels:
– The thoracic duct
– The right lymphatic duct
• Lymphatic organs are divided into primary and secondary
organs
• Primary organs include red bone marrow and thymus
• Secondary lymphatic organs and tissues Lymph nodes,
Spleen, Lymphatic nodules
• B-lymphocytes mature in the Bone marrow
• T-lymphocytes mature in the Thymus
• Lymph nodes are small, round or oval structures located
along the pathways of lymph vessels