The Large Intestine
• Terminal portion of the GI tract
• 1.5 m long and 6.5 cm in dm
• Extends from the ileum to the anus
• Attached to the posterior abdominal wall by its mesocolon
• Completion of absorption
• Production of certain vitamins
• Formation and expulsion of feces
Functions of the Large intestine
• Haustral churning, peristalsis, and mass peristalsis drive the contents of the colon into the rectum
• Bacteria in the large intestine convert proteins to amino acids, break down amino acids & produce some B vitamins and vitamin K
• Absorbing some water, ions, and vitamins
• Forming feces
• Defecating (emptying the rectum)
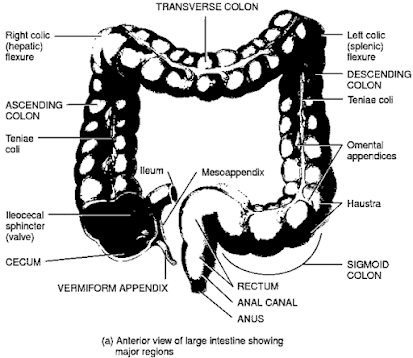
Large intestine Regions
•Cecum
•Colon
• Rectum
•Anal canal
Anatomy of large Intestine
• Ileocecal sphincter
– Opening from the ileum into the large intestine
– Guarded by a fold of mucous membrane
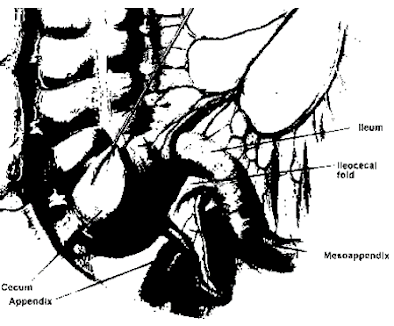
• Cecum
– Hanging inferior to the ileocecal valve is the cecum
– Small pouch about 6 cm long
• Appendix or vermiform appendix
– Twisted, coiled tube
– Attached to the cecum
• Mesoappendix
– The mesentery of the appendix
– Attaches the appendix to the inferior part of the mesentery of the ileum
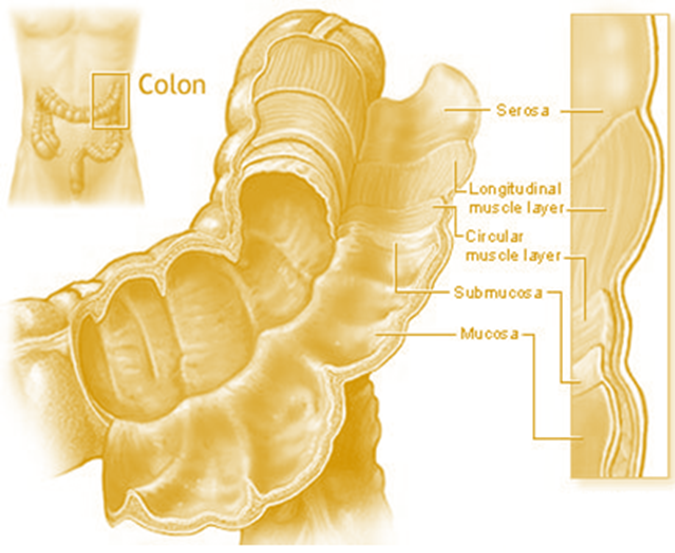
Colon
• Colon is divided into:
– Ascending (retroperitoneal)
– Transverse
– Descending (retroperitoneal)
– Sigmoid portion
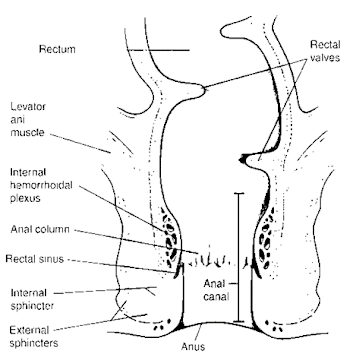
Rectum
• The last 20 cm of the GI tract
• Lies anterior to the sacrum & coccyx
• The terminal 2–3 cm – anal canal
• The mucous membrane of the anal canal is arranged in longitudinal folds called anal columns – contain a network of arteries and veins
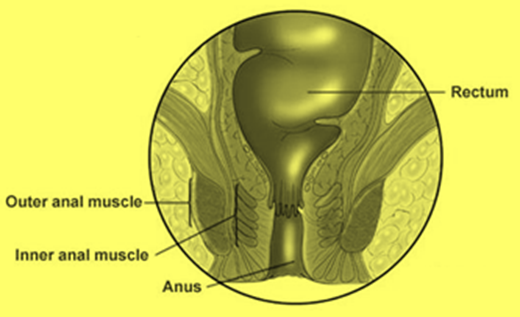
Anus
• The opening of the anal canal to the exterior, called the anus
• Anus – guarded by:
– Internal anal sphincter of smooth muscle (involuntary)
– External anal sphincter of skeletal muscle (voluntary)
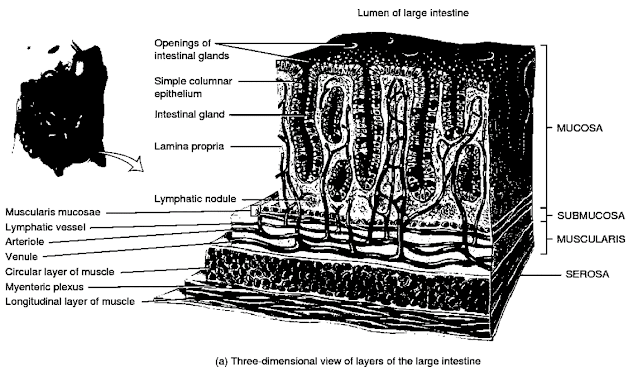
Histology of Large Intestine
• Typical four layers found in the rest of the GI tract: mucosa, submucosa, muscularis, and serosa
Histology of Large Intestine – Mucosa
• Consists of simple columnar epithelium
• Lamina propria (areolar connective tissue)
• Muscularis mucosae (smooth muscle)
• The epithelium contains: absorptive and goblet cellslocated in long, straight, tubular intestinal glands (crypts of Lieberkühn)
• Solitary lymphatic nodules are present
• No circular folds or villi (Small intestine contains)
• Microvilli are present on the absorptive cells
Sub mucosa
• Consists of areolar connective tissue
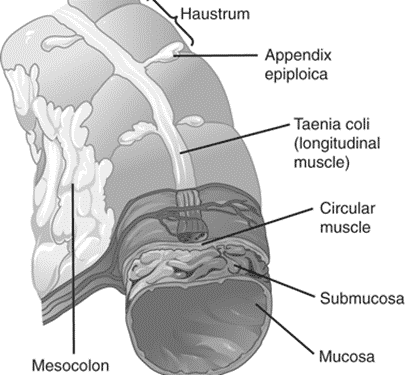
Muscularis
• Consists of:
– External layer of longitudinal smooth muscle
– Internal layer of circular smooth muscle
Serosa
– Part of the visceral peritoneum
– Small pouches of visceral peritoneum filled with fat are attached to teniae coli and are called omental (fatty) appendices
• Teniae coli
– Portions of the longitudinal muscles are thickened and
forms three conspicuous bands
– Run most of the length of the large intestine
• Haustra
– Tonic contractions of the bands gather the colon into a series of pouches
– give the colon a puckered appearance
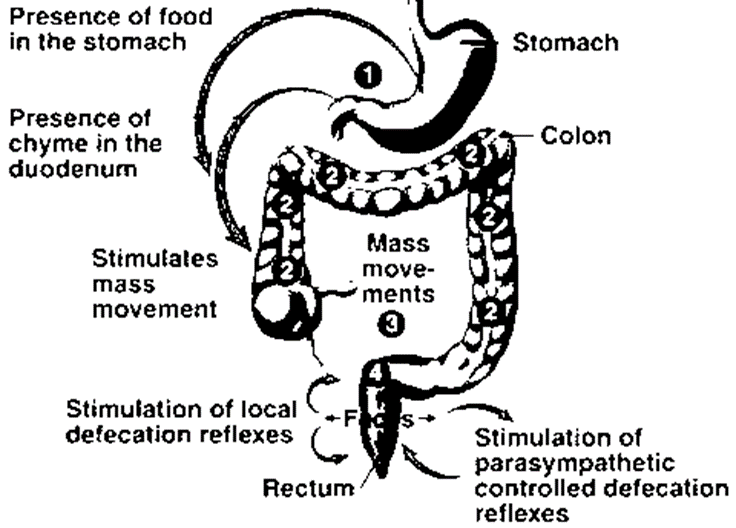
Mechanical Digestion in Large Intestine
• The passage of chyme from the ileum into the cecum is regulated by the action of the ileocecal sphincter
• Immediately after a meal, a gastroileal reflex intensifies peristalsis in the ileum
• Forces any chyme into the cecum
• Gastrin also relaxes the sphincter
• Movements of the colon begins
– Haustral churning: contraction and relaxation of haustral segments
– Peristalsis: rhythmic contraction
– A final type of movement is mass peristalsis – begins at middle of the transverse colon
• Drives the contents of the colon into the rectum
Chemical Digestion in Large Intestine
• Final stage of digestion occurs in the colon
• Mucus is secreted by the glands of the large intestine, but no enzymes are secreted
• Chyme is prepared for elimination by the action of bacteria
• Bacteria ferment any remaining carbohydrates and release hydrogen, carbon dioxide, and methane gases
• Bacteria also convert any remaining proteins to amino acids
• Break down the AA : Indole, skatole, hydrogen sulfide, and fatty acids
• Some of the indole and skatole is eliminated in the feces
• Rest is absorbed and transported to the liver
• Converted to less toxic compounds and excreted in the urine
• Bacteria also decompose bilirubin to simpler pigments
• Stercobilin (Pigment) gives feces their colour
Absorption and Feces Formation in the Large intestine
• Chyme remains in the large intestine for 3–10 hours
• Become solid or semisolid because of water absorption – feces
• Chemically consist of:
– Water
– Inorganic salts
– Sloughed-off epithelial cells from the mucosa of GIT
– Bacteria & products of bacterial decomposition
– Unabsorbed digested materials
– Indigestible parts of food
• Large intestine also absorbs water, ions including sodium and chloride, and some vitamins
Defecation Reflex
Phages of Digestion
Digestive activities occur in 3 overlapping phases:
Phase 1: Cephalic phase
Phase 2: Gastric phase
Phase 3: Intestinal phase
Cephalic Phase of Digestion
• The smell, sight, thought, or initial taste of food activates neural centers in the cerebral cortex, hypothalamus, and brain stem
• The brain stem then activates the facial (VII), glossopharyngeal (IX), and vagus (X) nerves
• The facial and glossopharyngeal nerves stimulate the salivary glands to secrete saliva
• The vagus nerves stimulate the gastric glands to secrete gastric juice
• The purpose of the cephalic phase of digestion is to prepare the mouth and stomach for food that is about to be eaten
Gastric Phase of Digestion
• Begins once food reaches the stomach
1) Neural Regulation
• Nerve impulses cause waves of peristalsis and continue to stimulate the flow of gastric juice from gastric glands
• The peristaltic waves mix the food with gastric juice
• Waves become strong enough – gastric emptying
• The pH of the stomach chyme & distension of the stomach decreases – gastric juice secretion suppresssed
2) Hormonal Regulation
• Stimulates gastric glands to secrete large amounts of gastric juice
• Strengthens the contraction of the LES to prevent reflux of acid chyme into the esophagus
• Increases motility of the stomach
• Relaxes the pyloric sphincter – promotes gastric emptying.
• Gastrin secretion is inhibited (pH drop below 2.0)
Intestinal Phase of Digestion
• Begins once food enters the small intestine
• Intestinal phase have inhibitory effects – slow the exit of chime from the stomach
• This prevents the duodenum from being overloaded
• Promote the continued digestion of foods that have reached the small intestine
• These activities of the intestinal phase of digestion are regulated by neural and hormonal mechanisms
Intestinal Phase of Digestion – Neural Regulation
• Distension of the duodenum by the presence of chyme causes the enterogastric reflex
• Stretch receptors in the duodenal wall send nerve impulses to the medulla oblongata
• Inhibit parasympathetic stimulation and stimulate the sympathetic nerves to the stomach
• As a result, gastric motility is inhibited & decreased gastric emptying
Intestinal Phase of Digestion – Hormonal Regulation
Cholecystokinin (CCK)
• Stimulates secretion of pancreatic juice
• Slows gastric emptying
• Produces satiety by acting on the hypothalamus in the brain
• Promotes normal growth and maintenance of the pancreas
Secretin
• Stimulates the flow of pancreatic juice that is rich in bicarbonate
• Buffer the acidic chyme that enters the duodenum
• Inhibits secretion of gastric juice
Also, Visit: The Small Intestine