Chronic inflammation

Objective
At the end of this PDF, student will be able to
• Define ‘chronic inflammation’
• Explain the causes of chronic inflammation
• Describe the general features of chronic inflammation
• Describe the pathogenesis granulomatous inflammation
Chronic inflammation
Chronic inflammation is defined as prolonged process in which tissue destruction and inflammation occur at the same time
Chronic inflammation – Causes
1. Chronic inflammation following acute inflammation:
• Prolonged acute inflammation
• Tissue destruction is extensive
• The bacteria survive & persist in small numbers at the site of acute inflammation
e.g. Osteomyelitis, pneumonia terminating in lung abscess
2. Recurrent attacks of acute inflammation:
• Repeated attacks of acute inflammation
• Culminate in chronicity of the process
e.g. – Recurrent urinary tract infection leading to chronic pyelonephritis
– Repeated acute infection of gallbladder leading to chronic cholecystitis
3. Chronic inflammation starting de novo:
• Infection with organisms of low pathogenicity is chronic
e.g. infection with Mycobacterium tuberculosis.
General features of chronic inflammation
Mononuclear cell infiltration
Infiltration of chronic inflammatory lesions
• Phagocytes – circulating monocytes, tissue macrophages, epithelioid cells, multinucleated giant cells
• Lymphoid cells
• Chemotactic factors and adhesion molecules for continued infiltration of macrophages
• Local proliferation of macrophages
• Longer survival of macrophages at the site of inflammation
Tissue destruction or necrosis
• Brought about by activated macrophages
• Release a variety of biologically active substances
E.g. protease, elastase, collagenase, lipase, reactive oxygen radicals, cytokines (IL-1, IL-8, TNF-α), nitric oxide, angiogenesis growth factor
Proliferative changes
• Result of necrosis
• Proliferation of small blood vessels and fibroblasts is
• Formation of inflammatory granulation tissue
• Healing by fibrosis and collagen laying
Systemic effects of chronic inflammation
• Fever: mild fever, often with loss of weight and weakness
• Anaemia
• Leucocytosis
• ESR: elevated in all cases
• Amyloidosis: Long-term cases of chronic suppurative Inflammation – secondary systemic (AA) amyloidosis
Types of chronic inflammation
Non-specific
• Irritant substance – nonspecific chronic inflammatory
• Formation of granulation tissue
• Healing by fibrosis (chronic osteomyelitis, chronic ulcer)
Specific
Injurious agent causes a characteristic histologic tissue response
e.g. tuberculosis, leprosy, syphilis
Granulomatous inflammation
Granuloma
• A tiny lesion about 1 mm in diamter
• Comprises of epitheloid cells in the centre & lymphoid in the periphery
• Contains gaint cells
• Associated with necrosis & fibrosis
• Proliferation of fibroblast in the periphery
• Due to presence of micro organism
e.g. Mycobacterium tuberculosis
– Poorly digestible
– Cell mediated immune response
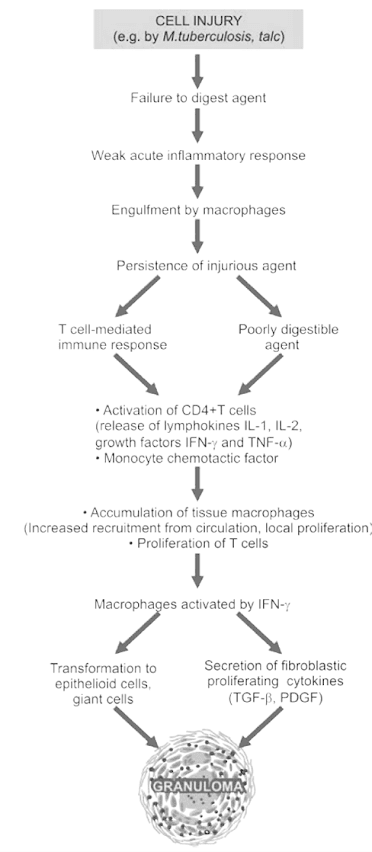
Pathogenesis of granulomatous inflammation
• Type IV hypersensitivity reaction
• Engulfment by macrophages
• Presentation of microbes to CD4+ T cells
• Activation of T-cells
• Cytokines
Composition of Granuloma
• Epithelioid cells
• Multinucleate giant cells
• Lymphoid cells
• Necrosis
• Fibrosis
Summary
• Chronic inflammation is defined as prolonged process in which tissue destruction and inflammation occur at the same time
• Chronic inflammation may occur due to prolonged and recurrent attack of acute inflammation or may start de novo
• Chronic inflammation is characterized by mononuclear cell infiltration, proliferation and necrosis
• Granulomatous inflammation occur by proliferation of fibroblast in the periphery due to presence of micro organism
FAQs
How long does chronic inflammation typically last?
Chronic inflammation can persist for months or even years, depending on the underlying causes and individual factors.
What are the common symptoms of chronic inflammation?
Common symptoms include fatigue, pain, swelling, and sometimes, a general feeling of unwellness.
Can chronic inflammation be reversed?
Yes, in many cases, adopting a healthier lifestyle and addressing the underlying causes can help reduce and reverse chronic inflammation.
Are there natural ways to reduce chronic inflammation?
Yes, incorporating an anti-inflammatory diet, regular exercise, and stress management techniques can be effective in reducing chronic inflammation.
How is granulomatous inflammation diagnosed and treated?
Diagnosis involves various tests, such as imaging and biopsies. Treatment depends on the underlying cause and may involve medications or other therapies. Early detection is crucial for effective management.