Anti-fungal antibiotics
•
Important
group
•
Two
classes- polyenes and griseofulvin
•
Polyenes-
complex antifungal antibiotics isolated from soil bacteria of the genus Streptomyces
•
Contain
a system of conjugated double bonds in macrocyclic lactone rings
•
Different
from erythromycin type structures (macrolides)
•
Larger
and contain the conjugated -ene system of double bonds- called polyenes
•
Clinically
useful polyenes- two groups- on the basis of size of macrolide ring
•
26-membered–ring
polyenes, such as natamycin (pimaricin) form one group
•
38-membered
macrocycles, such as amphotericin B and nystatin, form other group
•
Number
of double bonds in the macrocyclic ring differs also
•
Natamycin,
the smallest macrocycle, is a pentaene;
•
Nystatin
is a hexaene; and
•
Amphotericin
B is a heptaene
•
polyenes
have no activity against bacteria, rickettsia, or viruses
•
Highly
potent, broad-spectrum antifungal agents
•
Use of
the polyenes for the treatment of systemic infections is limited
•
toxicities
of the drugs,
•
Low
water solubilities, and
•
poor
chemical stabilities
•
Amphotericin
B, the only polyene useful for the treatment of serious systemic infections,
must be solubilized with a detergent
•
Other
polyenes are indicated only as topical agents for superficial fungal infections
Mechanism of action
•
In
three-dimensional shape,
•
a
barrel-like nonpolar structure capped by a polar group (sugar)
•
penetrate
the fungal cell membrane, acting as “false membrane components,”
•
bind
closely with ergosterol,
•
causing
membrane disruption,
•
cessation
of membrane enzyme activity, and
•
loss of
cellular constituents, especially potassium ions
Amphotericin B
•
Purified
from the fermentation beer of a soil culture of the actinomycete Streptomyces
nodosus, which was isolated in Venezuela
•
first
isolate from the streptomycete was a separable mixture of two compounds,
designated amphotericins A and B
•
In test
cultures, compound B proved to be more active, and this is the one used
clinically
•
Amphotericin
B is believed to interact with membrane sterols (ergosterol in fungi) to
produce an aggregate that forms a transmembrane channel
•
Intermolecular
hydrogen bonding interactions among hydroxyl, carboxyl, and amino groups
stabilize the channel in its open form
•
Destroying
symport activity and allowing the cytoplasmic contents to leak out
•
This
explains the toxicity in human patients
•
Is an
amphoteric substance, with a primary amino group attached to the mycosamine
ring and a carboxyl group on the macrocycle
•
Forms
deep yellow crystals that are sparingly soluble in organic solvents but
insoluble in water
•
To
create a parenteral dosage form, amphotericin B is stabilized as a buffered
colloidal dispersion in micelles with sodium deoxycholate
•
Nearly
80% of patients treated with amphotericin B develop nephrotoxicity
•
Fever, headache,
anorexia, gastrointestinal distress, malaise, and muscle and joint pain are
common
•
Pain at
the site of injection and thrombophlebitis are frequent complications of
intravenous administration.
•
Drug
must never be administered intramuscularly.
•
Hemolytic
activity of amphotericin B may be a consequence of its ability to leach
cholesterol from erythrocyte cell membranes
•
For
fungal infections of the CNS (e.g., cryptococcosis), amphotericin B is mixed
with cerebrospinal fluid (CSF) that is obtained from a spinal tap
•
Drug is
supplied in various topical forms, including a 3% cream, a 3% lotion, a 3%
ointment, and a 100-mg/mL oral suspension
Nystatin
•
First
isolated in 1951 from a strain of the actinomycete Streptomyces noursei by
Hazen and Brown
•
very
slightly soluble in water and sparingly soluble in organic solvents
•
unstable
to moisture, heat, and light
•
aglycone
portion of nystatin is called nystatinolide
•
It
consists of a 38-membered macrolide lactone ring containing single tetraene and
diene moieties separated by two methylene groups
•
Aglycone
also contains eight hydroxyl groups, one carboxyl group, and the lactone ester
functionality
•
Entire
compound is constructed by linking the aglycone to mycosamine
•
not
absorbed systemically when administered by the oral route
•
It is
nearly insoluble under all conditions
•
It is
also too toxic to be administered parenterally and used only as a topical agent
•
Valuable
agent for the treatment of local and gastrointestinal monilial infections
caused by C. albicans and other Candida species
•
For the
treatment of cutaneous and mucocutaneous candidiasis, it is supplied as a
cream, an ointment, and a powder
•
Oral
tablets are used in the treatment of gastrointestinal and oral candidiasis
Natamycin
•
Polyene
antibiotic obtained from cultures of Streptomyces natalensis
•
consists
of a 26-membered lactone ring containing a tetraene chromophore,
•
an α,β-unsaturated
lactone carbonyl group, three hydroxyl groups, a carboxyl group, a trans epoxide,
and a glycosidically joined mycosamine
•
natamycin
is amphoteric
•
Mechanism-
26-membered–ring polyenes cause both potassium ion leakage and cell lysis at
the same concentration
•
whereas
the 38-membered–ring polyenes cause potassium leakage at low, fungistatic
concentrations and cell lysis at high, fungicidal concentrations
•
smaller
polyenes are fungistatic and fungicidal within the same concentration range
•
supplied
as a 5% ophthalmic suspension intended for the treatment of fungal
conjunctivitis, blepharitis, and keratitis
Griseofulvin
•
antibiotic
obtained from the fungus Penicillium griseofulvum
•
It was
isolated originally as a “curling factor” in plants
•
drug has
been used for many years for its antifungal action in plants and animals
•
In 1959,
griseofulvin was introduced into human medicine for the treatment of tinea
infections by the systemic route
•
example
of a rare structure in nature, a spiro compound
•
compound
is a white, bitter, heat-stable powder or crystalline solid
•
sparingly
soluble in water but soluble in alcohol and other nonpolar solvents
•
used for
a long time for the systemically delivered treatment of refractory ringworm
infections of the body, hair, nails, and feet
•
caused
by species of dermatophytic fungi including Trichophyton, Microsporum
and Epidermophyton
•
Griseofulvin
neither possesses antibacterial activity nor is effective against P.
obiculare, the organism that causes tinea versicolor
•
most
common ones are allergic reactions such as rash and urticaria, gastrointestinal
upset, headache, dizziness, and insomnia
•
oral
bioavailability of griseofulvin is very poor
•
compound
is highly lipophilic with low water solubility
•
Several
structural derivatives have been synthesized, but they have failed to improve
absorption
•
best
advice that the pharmacist can give a patient who is about to use griseofulvin
is to take the drug with a fatty meal
Synthetic anti-fungal agents
•
Clotrimazole,
Econazole, Butoconazole, Oxiconazole Tioconozole Ketoconazole, Terconazole,
Itraconazole, Fluconazole, Naftifine hydrochloride
•
Synthesis-
Miconazole, Tolnaftate
Azole Antifungal Agents
•
Possess
a unique mechanism of action
•
Can
achieve selectivity for the infecting fungus over the host
•
Can
treat infections ranging from simple dermatophytoses to life-threatening, deep
systemic fungal infections
•
First
members of the class were highly substituted imidazoles, such as clotrimazole
and miconazole
•
Structure–activity
studies revealed that the imidazole ring could be replaced with a bioisosteric
1,2,4-triazole ring without adversely affecting the antifungal properties of
the molecule
Spectrum of activity
•
Azoles
tend to be effective against most fungi that cause superficial infections of
the skin and mucous membranes, including the dermatophytes such as Trichophyton,
Epidermophyton, and Microsporum spp. and yeasts such as C.
albicans
•
On the
other hand, they also exhibit activity against yeasts that cause systemic
infections, including C. immitis, C. neoformans, Paracoccidioides
brasiliensis, Petriellidium
boydii, B. dermatitidis,
and H. capsulatum
Azole Antifungal Agents- Mechanism of action
•
At
micromolar, the azoles are fungicidal
•
At
nanomolar, the azoles are fungistatic
•
Fungicidal
effect is clearly associated with damage to the cell membrane, with the loss of
essential cellular components such as potassium ions and amino acids
•
Fungistatic
effect is associated with inhibition of membrane-bound enzymes
•
A
cytochrome P450-class enzyme, lanosterol 14α-demethylase, is the likely target for the
azoles
•
Function
of lanosterol 14α-demethylase is to
oxidatively remove a methyl group from lanosterol during ergosterol
biosynthesis
•
Lanosterol
14α-demethylase is also required for mammalian
biosynthesis of cholesterol, and the azoles are known to inhibit cholesterol
biosynthesis
•
Higher
concentrations of the azoles are needed to inhibit the mammalian enzyme
•
Provides
selectivity for antifungal action
•
1,2,4-triazoles
appear to cause a lower incidence of endocrine effects and hepatotoxicity than
the corresponding imidazoles
•
Possibly
because of a lower affinity for the mammalian cytochrome P450 enzymes involved
Clotrimazole
•
Broad-spectrum
antifungal drug that is used topically for the treatment of tinea infections
and candidiasis
•
It
occurs as a white crystalline solid that is sparingly soluble in water but
soluble in alcohol and most organic solvents
•
It is a
weak base that can be solubilized by dilute mineral acids
•
Extremely
stable, with a shelf life of more than 5 years
•
Effective
against various pathogenic yeasts and
•
Reasonably
well absorbed orally, extensively protein bound
•
Not
considered suitable for the treatment of systemic infections
Econazole
•
It is
only slightly soluble in water and most organic solvents
•
Used as
a 1% cream for the topical treatment of local tinea infections and cutaneous
candidiasis
Butoconazole
•
Extremely
broad-spectrum antifungal drug that is specifically effective against C.
albicans
•
It is
intended for the treatment of vaginal candidiasis- 2% of butoconazole nitrate
in the form of cream
Oxiconazole
•
It is
used in cream and lotion dosage forms in 1% concentration for the treatment of
tinea pedis, tinea corporis, and tinea capitis
Tioconazole
•
Used for
the treatment of vulvovaginal candidiasis
•
A
vaginal ointment containing 6.5% of the free base is available
•
More
effective against Torulopsis glabrata than are other azoles
Miconazole
•
Occurs
as white crystals that are sparingly soluble in water and most organic solvents
•
The free
base is available in an injectable form, solubilized with polyethylene glycol
and castor oil, and intended for the treatment of serious systemic fungal
infections
•
Like
candidiasis, coccidioidomycosis, cryptococcosis, petriellidiosis, and
paracoccidioidomycosis
•
thrombophlebitis,
pruritus, fever, and gastrointestinal upset are relatively common side effects
Ketoconazole
•
broad-spectrum
imidazole antifungal agent that is administered orally for the treatment of
systemic fungal infections
•
It is a
weakly basic compound that occurs as a white crystalline solid that is very
slightly soluble in water
•
primary
route of excretion is enterohepatic
•
It is
estimated to be 95% to 99% bound to protein in the plasma
•
Hepatotoxicity-
most serious adverse effect
•
known to
inhibit cholesterol biosynthesis in both mammals and fungi
•
High
doses have also been reported to lower testosterone and corticosterone levels
•
Ketoconazole
is a racemic compound, consisting of the cis-2S,4R and cis-2R,4S
isomers
•
trans-isomers, 2S,4S and 2R,4R,
are much less active
•
recommended
for the treatment of the following systemic fungal infections: candidiasis
(including oral thrush and the chronic mucocutaneous form), coccidioidomycosis,
blastomycosis, histoplasmosis, chromomycosis, and paracoccidioidomycosis
•
It is
also used orally to treat severe refractory cutaneous dermatophytic infections
not responsive to topical therapy or oral griseofulvin
•
antifungal
actions of ketoconazole and the polyene antibiotic amphotericin B are reported
to antagonize each other
•
used
topically in a 2% concentration in a cream and in a shampoo for the management
of cutaneous candidiasis and tinea infections
Terconazole
•
Triazole
derivative that is used exclusively for the control of vulvovaginal moniliasis
caused by C. albicans and other Candida species
•
It is
available in creams containing 0.4% and 0.8% of the free base intended for
7-day and 3-day treatment periods, respectively
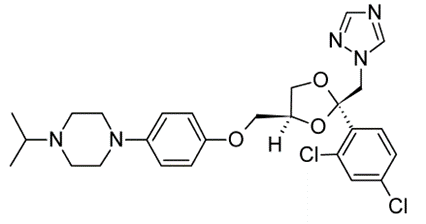
Itraconazole
•
Unique
member of the azole class that contains two triazole moieties in its structure
•
A weakly
basic 1,2,4-triazole and a non-basic 1,2,4-triazol-3-one
•
orally
active, broad-spectrum antifungal agent and important alternative to
ketoconazole
•
An
acidic environment is required for optimum solubilization and oral absorption
•
Food
greatly enhances the absorption of itraconazole, nearly doubling its oral
bioavailability
•
drug is
avidly bound to plasma proteins (nearly 99% at clinically effective
concentrations) and extensively metabolized in the liver
•
Only one
of the numerous metabolites, namely 1-hydroxyitraconazole, has significant
antifungal activity
•
terminal
elimination half-life of itraconazole ranges from 24 to 40 hours
•
Used for
the treatment of systemic fungal infections including blastomycosis,
histoplasmosis (including patients infected with [HIV]),
•
nonmeningeal
coccidioidomycosis, paracoccidioidomycosis, and sporotrichosis
•
It may
also be effective in the treatment of pergellosis, disseminated and deep organ
candidiasis, coccidioidal meningitis, and cryptococcosis
•
Unlike
ketoconazole, it is not hepatotoxic and does not cause adrenal or testicular
suppression in recommended therapeutic doses
Fluconazole
•
Water
soluble bis-triazole with broad-spectrum antifungal properties
•
Suitable
for both oral and intravenous administration as the free base
•
Excellent
bioavailability in both tablet and suspension dosage forms
•
Presence
of two weakly basic triazole rings in the molecule confers sufficient aqueous
solubility to balance the lipophilicity of the 2,4-difluorophenyl group
•
Has a
relatively long elimination half-life, ranging from 27 to 34 hours
•
It
penetrates well into all body cavities, including the CSF
•
Little or
no hepatic metabolism and is excreted substantially unchanged in the urine
•
Plasma
protein binding of fluconazole is less than 10%
•
Inhibition
of cytochrome P450 oxidases by fluconazole can give rise to clinically
significant interactions involving increased plasma levels of cyclosporine,
phenytoin, and the oral hypoglycemic drugs
•
Recommended
for the treatment and prophylaxis of disseminated and deep organ candidiasis
•
It is
also used to control esophageal and oropharyngeal candidiasis
•
Agent of
choice for the treatment of cryptococcal meningitis and for prophylaxis against
cryptococcosis in AIDS patients
Naftifine Hydrochloride
•
White
crystalline powder that is soluble in polar solvents such as ethanol and
methylene chloride
•
It is
supplied in a 1% concentration in a cream and in a gel for the topical
treatment of ringworm, athlete’s foot, and jock itch
•
Although
unapproved for these uses, naftifine has shown efficacy for treatment of
ringworm of the beard, ringworm of the scalp, and tinea versicolor
Tolnaftate
•
White
crystalline solid that is insoluble in water, sparingly soluble in alcohol, and
soluble in most organic solvents
•
compound,
a thioester of β-naphthol, is fungicidal
against dermatophytes, such as Trichophyton, Microsporum, and Epidermophyton
spp., that cause superficial tinea infections
•
Available
in a concentration of 1% in creams, powders, aerosols, gels, and solutions for
the treatment of ringworm, jock itch, and athlete’s foot
•
Shown to
act as an inhibitor of squalene epoxidase
•
in
susceptible fungi
Miconazole- Synthesis
Tolnaftate- Synthesis
2-naphthol and
thiophosgene to make a monosubstituted product of thiophosgene, which is then
reacted with N-methyl-3-toluidine to give the desired tolnaftate